




Cases 4-10 Discussion
Case 4 and Case 4 Comparison--to view HINT annotations, return to the Case page
Further Explanation:
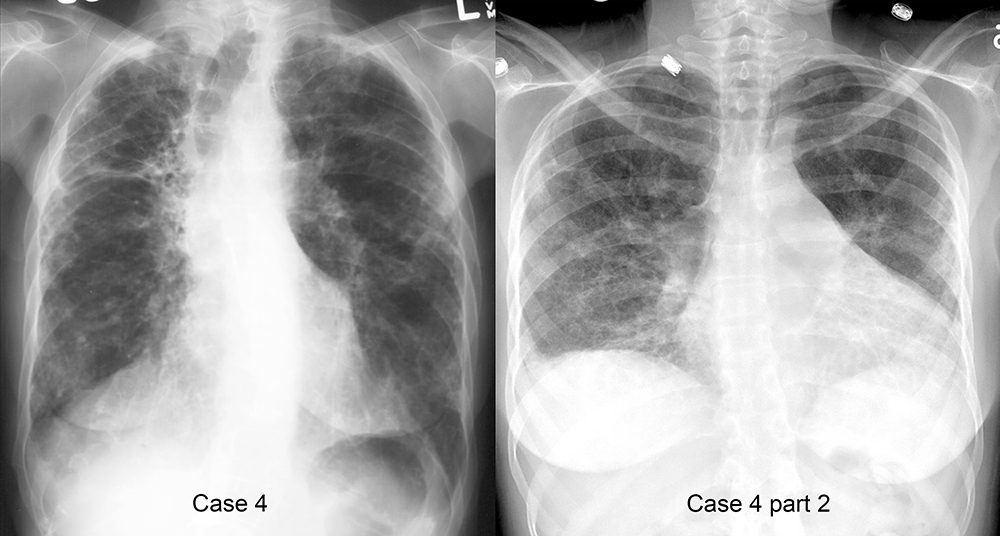
Case 4--
Hint 1: There are too many markings in the periphery of the lung, especially in the upper lungs, with a linear or reticular pattern. There are also some small black areas the could represent cysts or honeycombing. This is suggestive of fibrosis, although other diagnoses are possible.
Hint 2: There are only 9 posterior ribs visible above the diaphragms (and the top-to-bottom diameter of the chest seems pretty close to the side-to-side diameter) suggesting overall low lung volumes. This could also go along with fibrosis, which generally produces restriction and retraction of the lung tissues.
Hint 3: The curved interface arching upward on the right is the minor fissure, which is too high in position and bowed upward more than normal. This also suggests volume loss involving the upper lobe, pulling the fissure upward. The combination of these findings (too many reticular markings in the peripheral and upper lungs with possible honeycombing, evidence of volume loss particularly in the upper lobes) is most consistent with a fibrotic process that favors upper lobes, such as sarcoidosis. Other possibilities would be silicosis or coal-workers pneumoconiosis, depending on the patient history.
Case 4 Comparison--
Hint 1: The cardiac silhouette is definitely enlarged, with the left side of the heart border touching the inner left ribcage. This could represent cardiomegaly or possibly pericardial fluid.
Hint 2: There are too many lung markings in the periphery and bases of the lungs. Many of these markings look reticular, but some are a bit more hazy. It may be difficult to always determine if opacities in the lung are alveolar or interstitial, but you need to decide what you think is predominant, and many lung diseases show a mixture of both.
Hint 3: The lowest posterior rib that is visible is rib 8, which indicates very low lung volumes. The top-to-bottom diameter of the lungs looks smaller than the side-to-side diameter. The combination of these findings (very low lung volumes, increased cardiac silhouette, and mostly reticular markings in the lung periphery and bases) suggests a fibrotic process that favors the lung bases, such as scleroderma, which can also produce a cardiomyopathy and enlargement of the heart. Scleroderma can also result in pericardial effusion, but it is rare for them to be very large. Alternatively, this could represent CHF with interstitial edema rather than fibrosis.
Cases 4-10 Discussion
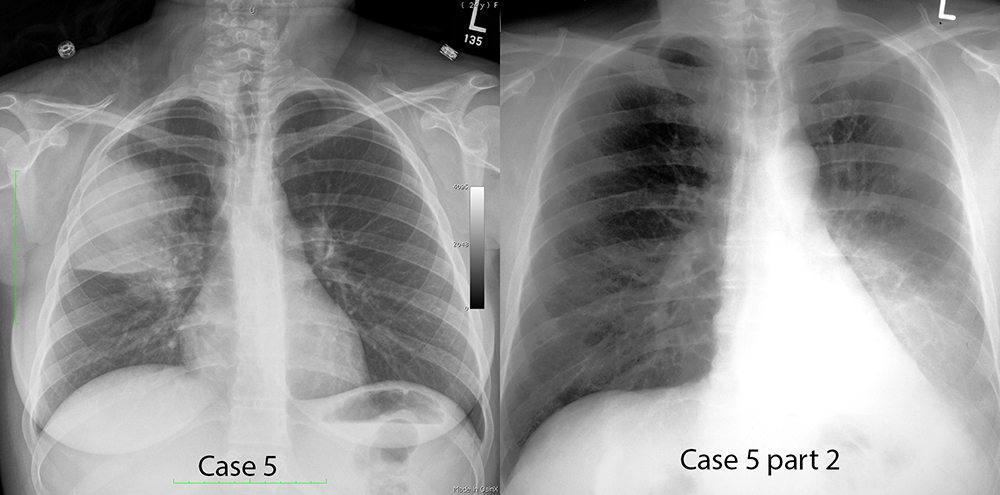
Case 5 and Case 5 Comparison
Further Explanation:
Case 5--
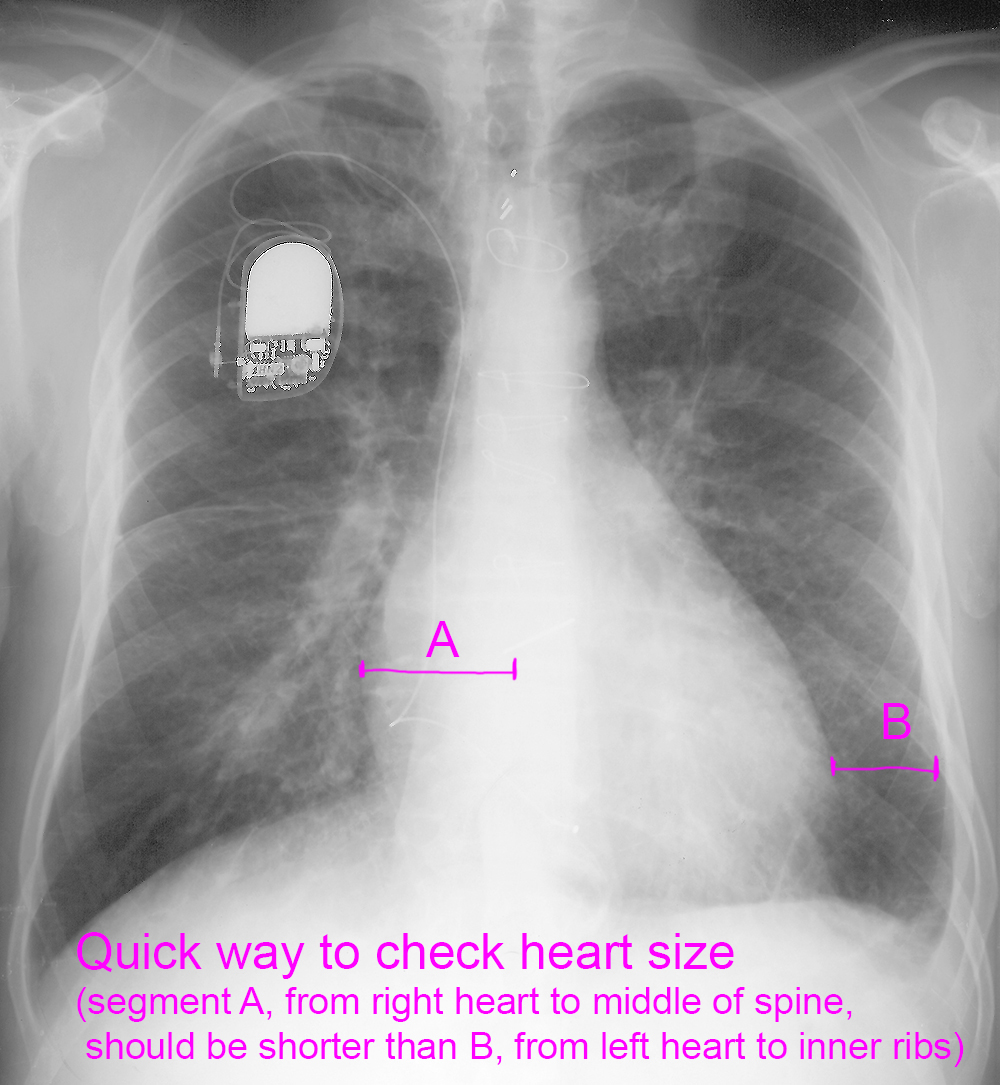
Hint 1: This heart is not enlarged, based on the standard measurements. This makes congestive heart failure very unlikely.
Hint 2: There is an opacity in the right mid to upper lung that has a hazy upper margin consistent with an alveolar filling process.
Hint 3: The bottom edge of the opacity is smooth and horizontal, indicating that the lower border of the process is limited by a fissure--the minor fissure in this case. The combination of these findings (no cardiomegaly, alveolar opacity above the minor fissure) is most consistent with a right upper lobe pneumonia. A pneumonia in the right LOWER lobe could be located at the same level in the chest, but would not have a sharp, smooth inferior border like this. A pneumonia in the right middle lobe would have a smooth UPPER border, not lower, since the middle lobe is located below the minor fissure.
Case 5 Comparison--
Hint 1: The heart is outlined in red, and appears shifted to the left. There is no part of the right heart border visible to the right of the spine.
Hint 2: The heart is not enlarged, bases on the standard measurements.
Hint 3: There is an ill-defined opacity in the lower left lung, with an alveolar appearance. It does NOT obscure the left heart border, indicating that it is not located anteriorly (where the heart is). This combination of findings (shift of heart to the left with alveolar opacity in the lower left chest not obscuring the heart border) is most consistent with a left lower lobe pneumonia that may be post-obstructive in nature. Regular pneumonias without obstruction do not typically cause volume loss and shift of the mediastinum. Volume loss with pneumonia can be seen in obstruction of the bronchi by such things as carcinoid, lung cancer, enlarged hilar nodes (as in TB, sarcoid, lymphoma) or aspirated foreign bodies. In this case, it was a left lower lobe lung cancer.
Cases 4-10 Discussion
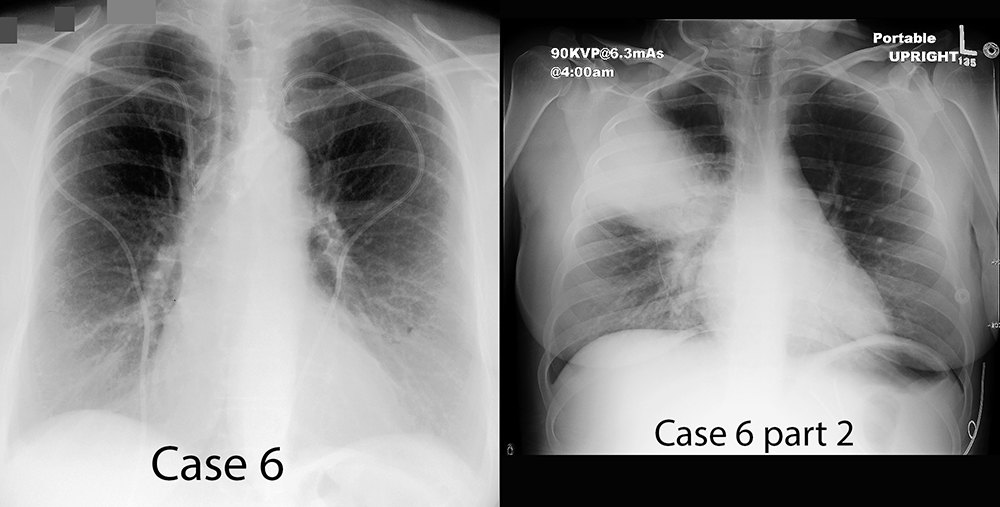
Case 6 and Comparison Case 6
Further Explanation:
Case 6-
Hint 1: There are bilateral central lines, indicated on the right in yellow and the left in green. Their tips are projecting along the right mediastinal border just above the smooth bulge of the right atrium.
Hint 2: The approximate likely location of the skin entry point is shown on each site in brown. This is not often easy to be sure about based on radiography alone. The approximate likely location of the vascular entry point is shown in blue, and should be determined by the position of the target vessels, most often the internal jugular or subclavian vein.
Hint 3: The approximate location of the upper venous structures is shown here. The exact position of these vessels can vary from one patient to another, particularly the course and crossing level of the left brachiocephalic vein. The combination of these findings (bilateral catheters that travel somewhat horizontally in the region of the medial clavicles and are directed downward along the right mediastinal border to terminate above the right atrium) is consistent with bilateral subclavian line placement in satisfactory position.
Case 6 Comparison-
Hint 1: This is the same patient we saw earlier with right upper lobe pneumonia, which has worsened, leading to placement of a central line to deliver intravenous antibiotics. The line position is indicated in green, and since it seems to be coming down from the right neck, rather than horizontally along the clavicle, it was likely intended to be in internal jugular line.
Hint 2: The expected position of a right IJ central line is shown in yellow, along with the expected location of pertinent venous structures. The patient's actual central line (green) is not following the expected path of a right internal jugular line.
Hint 3: The arterial structures in the region are shown in red, with the course of the patient's central line in green. The combination of these findings (central line coming down from the neck but in a position too far medial from the expected venous structures) is consistent with an arterial placement into the carotid artery instead of the IJ. This is an uncommon occurrence unless the patient is very ill, with poor cardiac output and poor oxygenation, since arterial blood is usually easily recognized at the time of line placement. This patient was hypotensive at the time the line was placed, which likely accounts for this complication.
Cases 4-10 Discussion
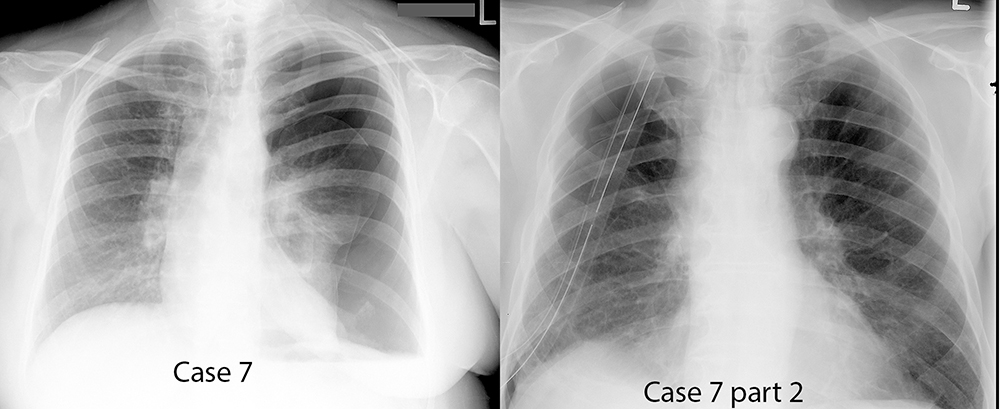
Case 7 and Case 7 Comparison
Further Explanation:
Case 7-
Hint 1: Curvilinear white lines are seen outlining the partly collapsed left upper and lower lobes, shown in blue.
Hint 2: There are no lung markings or vessels seen in the space outside the white lines on the left.
Hint 3: The heart is shifted to the left from its normal position, indicated in red. The combination of these findings (white lines with no lung markings beyond, and shift of the mediastinum away from the abnormal side) are consistent with a large left pneumothorax with concern for tension pneumothorax. Tension pneumothorax occurs when pressure is increased within the affected pleural space, causing severe lung collapse and pushing mediastinal structures away, which can lead to compression of venous structures and decreased cardiac output. This is a CLINICAL diagnosis, not a radiologic one, since different patients react differently to the same degree of mediastinal shift, but the findings in this case are dramatic enough to make tension pneumothorax likely.
Case 7 Comparison-
Hint 1: A curvlinear white pleural line is seen on the right, indicated in blue, with absence of lung markings above it.
Hint 2: A segment of the right posterolateral 5th rib is missing (indicated in yellow), and there are two relatively large caliber tubes projecting over the right hemithorax with end and side holes (indicated in green).
Hint 3: The heart is in normal position, with no shift to the left or right. The combination of these findings (white pleural line, missing rib. two tubes. no mediastinal shift) are most consistent with recent thoracotomy, small right pneumothorax, and two chest tubes, which are placed to drain pleural fluid and air post-operatively. The most likely reason for the presence of pneumothorax in this setting is that the tubes have been clamped for a period of time prior to their planned removal, with a chest radiograph obtained to see if there is still air leaking from the surgical site. In this case, the presence of a pneumothorax indicates ongoing air leak, and the tubes will likely returned to suction for another period of time before testing again and ultimate removal.
Cases 4-10 Discussion
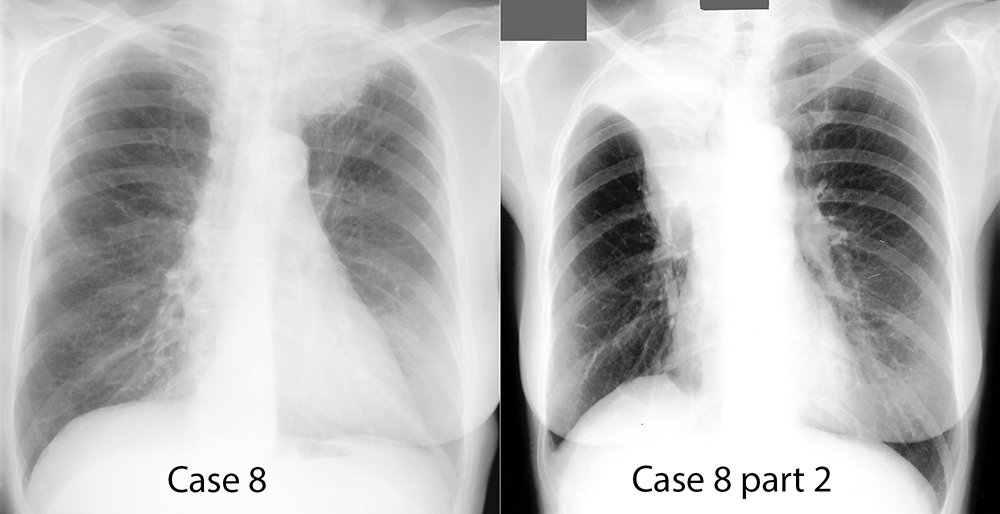
Case 8 and Case 8 Comparison
Further Explanation:
Case 8-
Hint 1: There is an opacity with a rather irregular margin projecting in the left lung apex, shown in red.
Hint 2: The vascular structures of the upper extremity pass through this region, including the subclavian artery (shown in red) and vein (shown in blue)
Hint 3: The structures of the brachial plexus (shown in green) also pass through this region. The findings in this case (large left apical mass) are most consistent with a Pancoast tumor, a lung cancer that can compress brachial vascular structures or neural structures, leading to upper extremity symptoms.
Case 8 Comparison-
Hint 1: There is an s-shaped interface in the right hemithorax, curving upward in its lateral portion, and downward near the hilum.
Hint 2: The cause of this shape is indicated in red (central hilar mass) and blue (collapsed distal lung).
Hint 3: The right hemidiaphragm is elevated and tented, shown in green. The combination of these findings (S-shaped interface with opacity above, elevated tented diaphragm) is most consistent with a central lung mass, such as a small cell lung carcinoma, with collapse of the distal lung, leading to elevation of the diaphragm due to collapse of the upper lobe.
Cases 4-10 Discussion
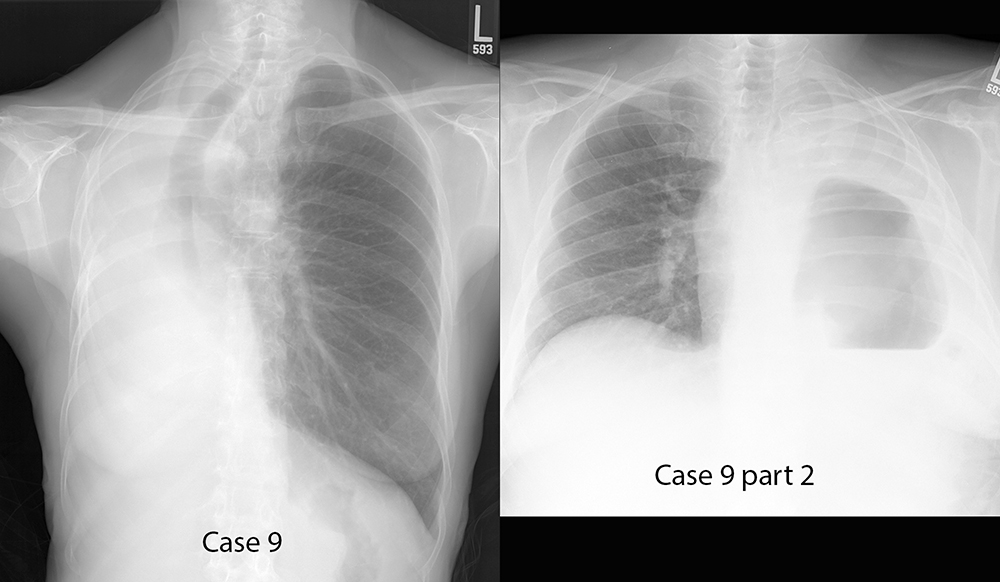
Case 9 and Case 9 Comparison
Further Explanation:
Case 9-
Hint 1: There is no aerated lung visible in the right hemithorax, which is completely opaque. The two things to consider are volume loss of the right lung or a space-occupying lesion such as a mass or effusion.
Hint 2: The position of the airway is indicated in yellow. The trachea and bronchi are pulled to the right, toward the abnormal opacity.
Hint 3: The heart is not well seen, and no cardiac structures are visible to the left of the spine. The likely position of the heart is indicated in red. The combination of these findings (right hemithorax opacity, right-ward shift of the airway and heart) are most consistent with right lung volume loss, which could be due to complete lung collapse or pneumonectomy (removal of the right lung). In this case, the history was of lung cancer and right pneumonectomy. When the entire lung is removed, the space it previously occupied must be filled. In this patient, the heart and mediastinum shifted far to the right to fill the space.
Case 9 Comparison-
Hint 1: In this case, the entire left lung is opaque with no normally aerated lung seen.
Hint 2: The heart appears to be in relatively normal position, based on the portion of the right atrium that remains to the right of the spine. The trachea is not deviated, but appears in relatively normal position.
Hint 3: The left hemithorax contains a large air-filled space with a flat bottom--an air fluid level. This is most consistent with upward displacement of the stomach due to volume loss. This patient also had a pneumonectomy but the space formerly occupied by the left lung was filled by gradual upward displacement of the diaphragm and movement of upper abdominal organs into the space. Different patients react differently to pneumonectomy, and different structures can move to fill the space formerly occupied by the lung.
Cases 4-10 Discussion
Case 10 and Case 10 Comparisons
Further Explanation:
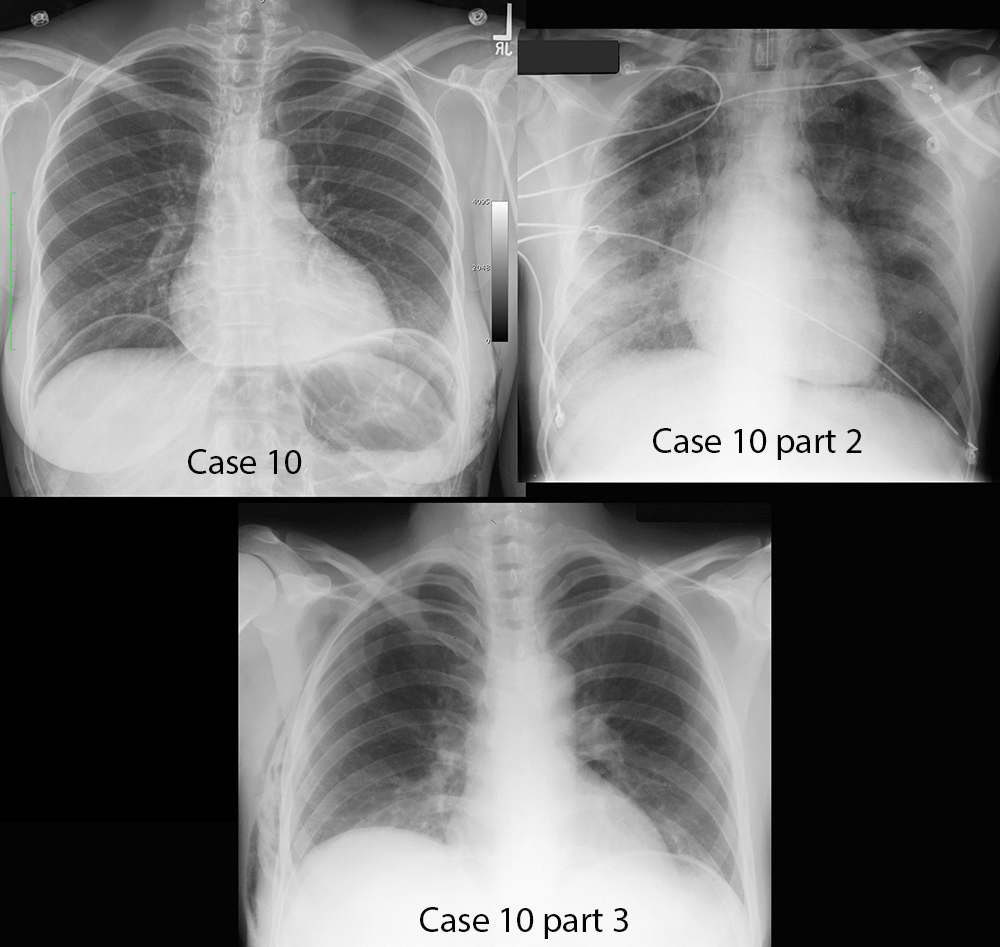
Case 10--
Hint 1: The green outlines show curvilinear white areas bilaterally that are thicker than the white pleural line of a pneumothorax, and are not in the typical location of pneumothorax in the upright position, which is in the apex.
Hint 2: Beneath the white lines are crescent-shaped areas of lucency without lung markings, shown here in blue. This lucent area appears to extend from one side of the upper abdomen to the other.
Hint 3: There are also abnormal lucencies in the lateral portions of the abdominal walls, outlined in blue. The combination of these findings (Curvilinear densities at the bases with lucency below and lucency in soft tissues) is most consistent with intraperitoneal air, which usually does not dissect along tissue planes into the abdominal wall. In this case, the patient had previous laparoscopic surgery, and air tracked from the abdominal incisions (through which gas is instilled into the peritoneal cavity to allow visualization and manipulation of organs) into the subcutaneous tissues of the abdomen and chest wall.
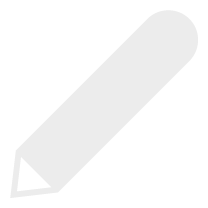
Case 10 Comparison 1-
Hint 1: This portable chest radiograph shows that there is a large caliber tube projecting over the upper trachea, outlined in green.
Hint 2: There is a slightly vague curvilinear density that runs along the left mediastinal border, outlined in blue.
Hint 3: There are subtle areas of lucency medial to the curvilinear density on the left, extending deep into the mediastinum, particularly between the aorta and pulmonary artery. There are also other streaky areas of lucency in other parts of the mediastinum. The combination of these findings (ET tube, streaky air outlining mediastinal structures) is consistent with air in the connective tissues of the mediastinum, pneumomediastinum. This can be caused by many conditions, but with an endotracheal tube in place, this could be due to lung damage from positive pressure ventilation, with air dissecting back from the lung into the mediastinum. Other causes include trauma to central airways or esophageal perforation.
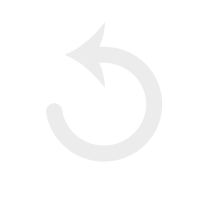
Case 10 Comparison 2-
Hint 1: There is air in the right lateral chest wall soft tissue, indicated in blue. There is no evidence of pneumothorax, pneumoperitoneum or pneumomediastinum.
Hint 2: Rib 8 is the lowest rib on the right seen above the diaphragm, indicating low lung volumes.
Hint 3: The heart is not enlarged. The combination of these findings (subcutaneous chest wall air with low lung volumes but no pneumothorax, pneumoperitonem or pneumomediastinum) should suggest other causes of subcutaneous emphysema NOT related to bowel perforation or pneumothorax, such as soft tissue infection. This is an emergency, as these types of infections can be rapidly progressive and can lead to extensive tissue damage and death if not treated promptly.