




Angiography
Introductory angiography image
Question 1:
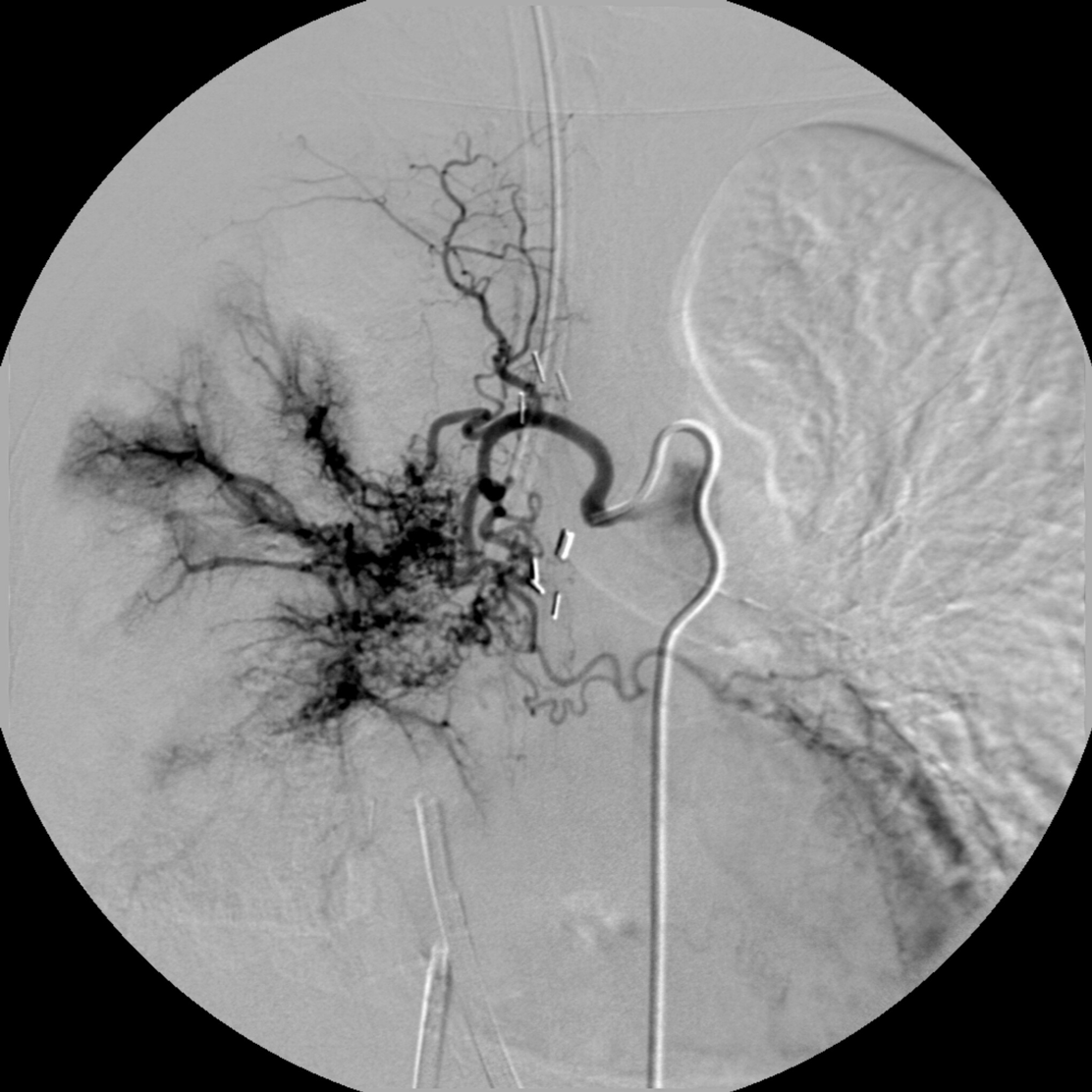
A 58 year-old female with history of hypertension and who is now status post-successful left renal stent placement by interventional radiology presents with worsening severe hypertension. Interventional radiology is consulted for diagnostic selective renal arteriography. What are the relevant imaged findings?
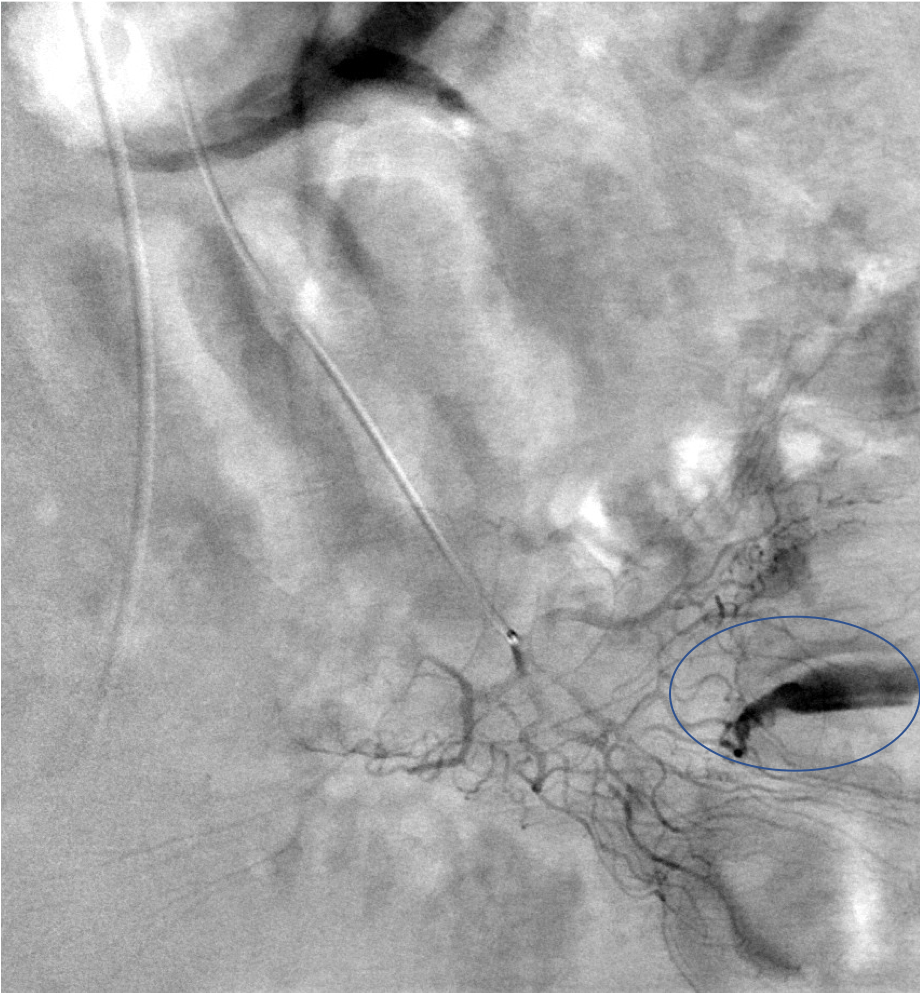
A diagnostic selective substraction left renal arteriographic image is obtained via a catheter placed within the origin of the left renal artery. A patent left renal stent is noted on diagnostic evaluation, with no evidence of stenosis or irregularity in the renal artery. However, multiple punctate sac-like aneurysms are noted throughout the kidney, particularly in the mid to peripheral renal arterial vasculature.

Question 2:
What is your diagnosis?
This patient who is also found to have an acutely elevated erythocyte sedimentation rate (ESR) on laboratory analysis likely has necrotizing arteritis. This is a condition that affects the medium and small arteries. As such, it occurs predominantly in the kidney (80%), liver (66%), and GI (51%) tract. Its findings on angiography include multiple sac- or fusiform-like microaneurysms, which are at an increased risk for rupture and associated hemorrhage. Infarcts may also be observed. The differential diagnosis for this angiographic appearance may represent underlying septic emboli, drug-related pathology or cryoglobulinemia. Management is immunosuppression.

Question 3:
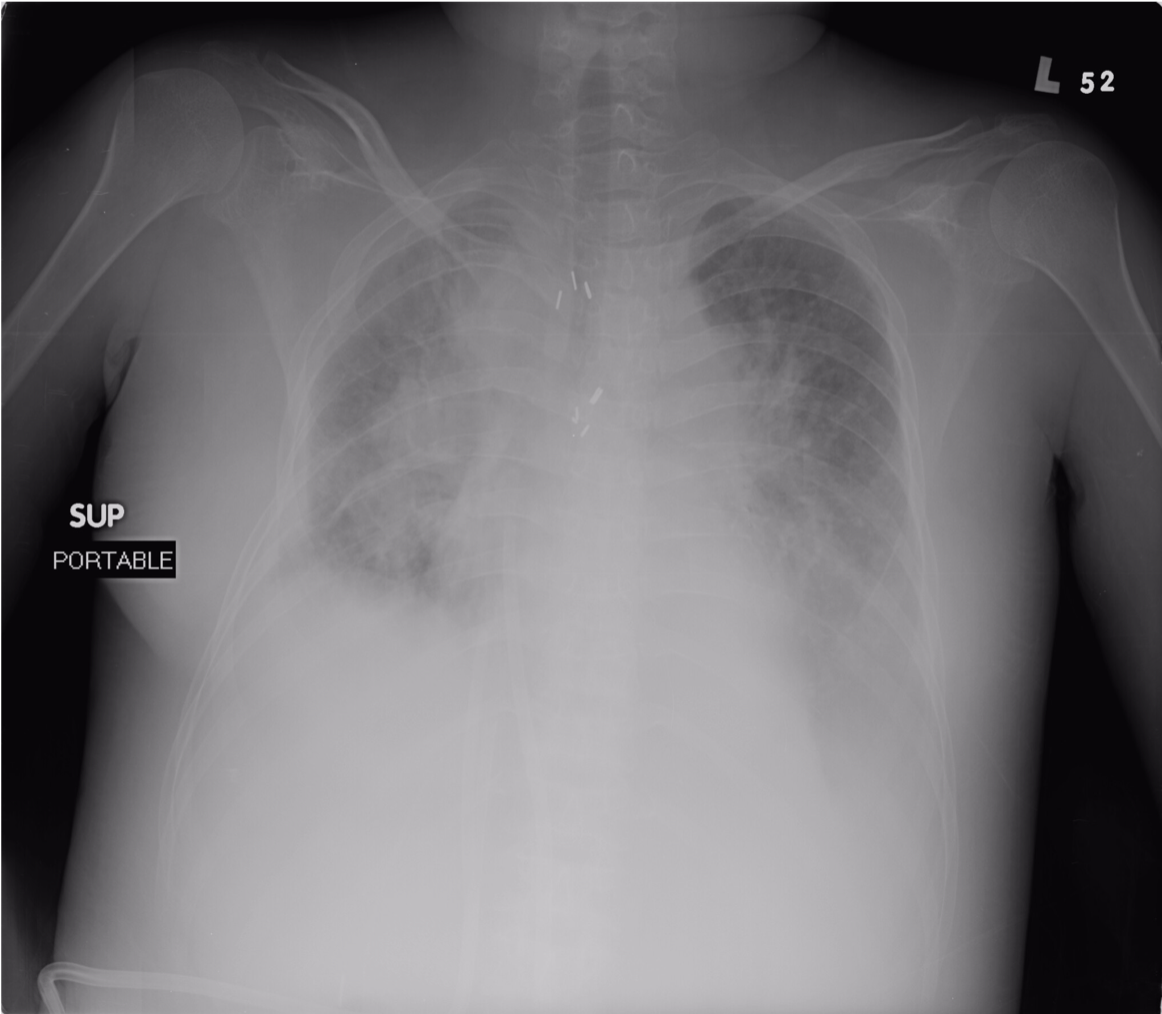
A 31 year old female with history of congenital protein-losing enteropathy, end-stage liver disease secondary to chronic TPN and acute renal failure presents with an acute episode of hemoptysis. What are the indications for involving interventional radiology in this patient’s care?
Interventional radiology is consulted when patients exhibit evidence of massive hemoptysis. This is defined as expectoration of blood measuring 300-600ml/24 hrs or 100 ml/day X 5 days. Alternatively, IR may be consulted if the episode of hemoptysis reflects an amount sufficient to provoke a life-threatening condition.
Question 4:
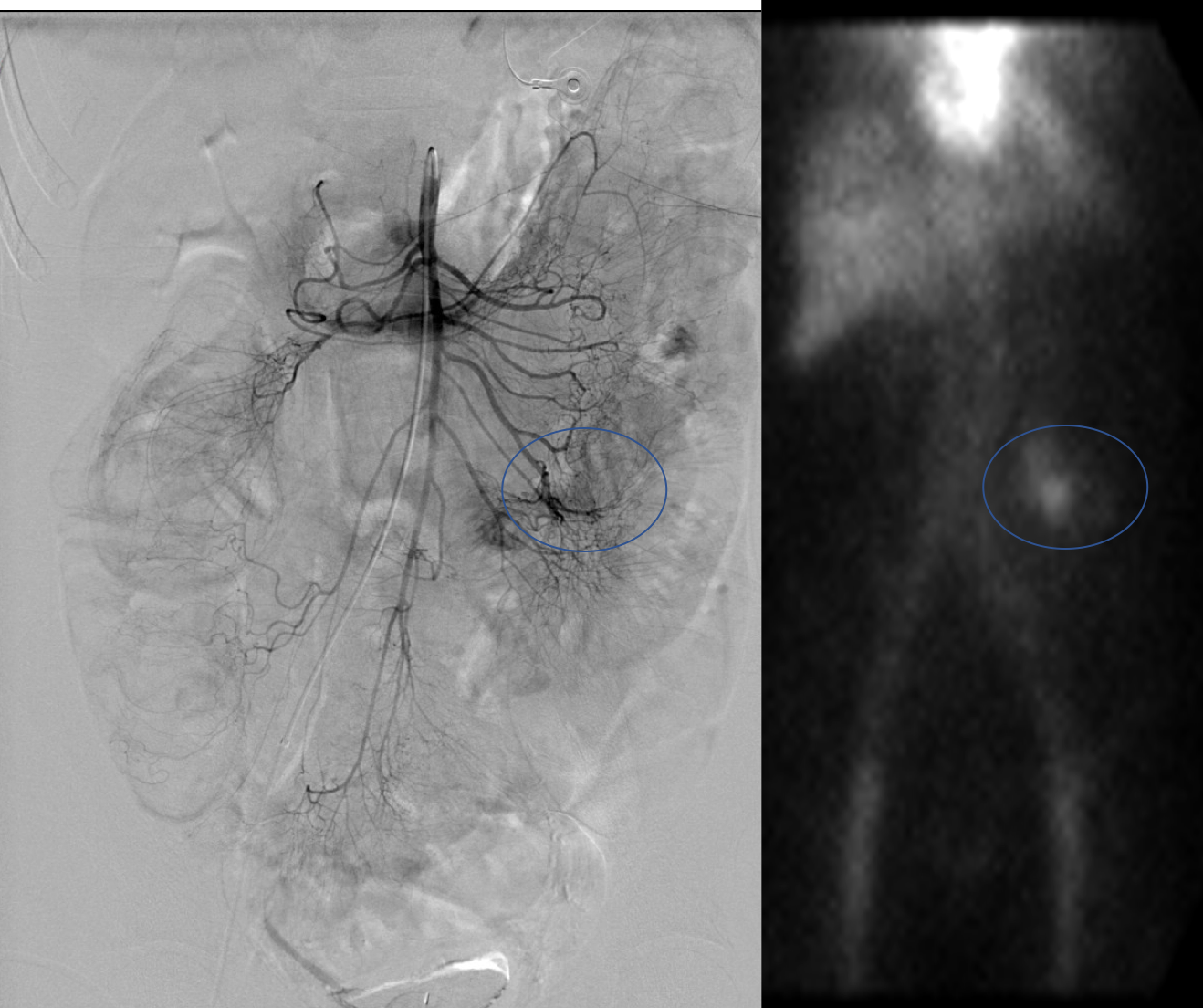
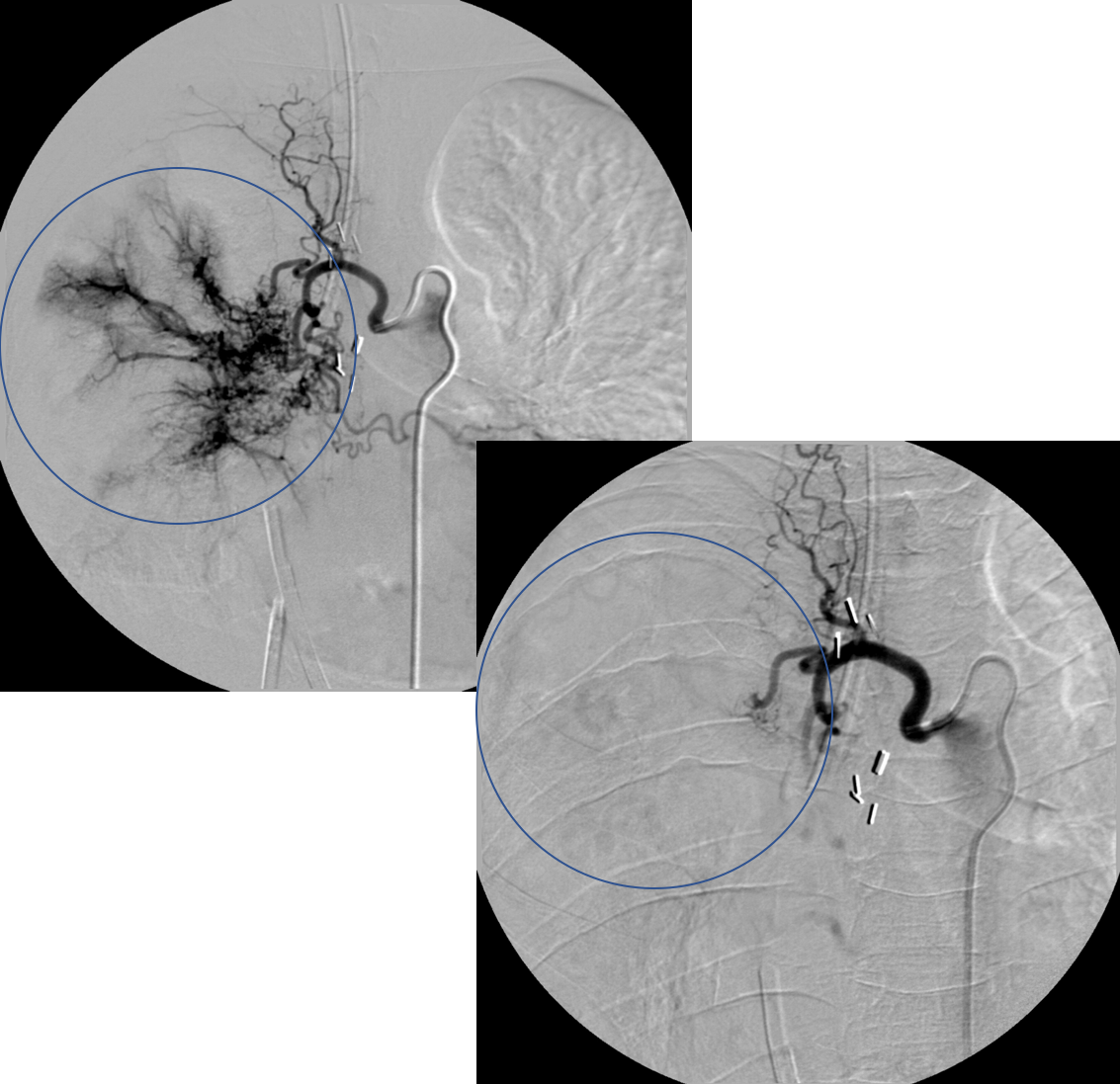
The patient is found to meet the the criteria for massive hemoptysis. IR is consulted for a diagnostic bronchial arteriogram. What is depicted in the associated image?
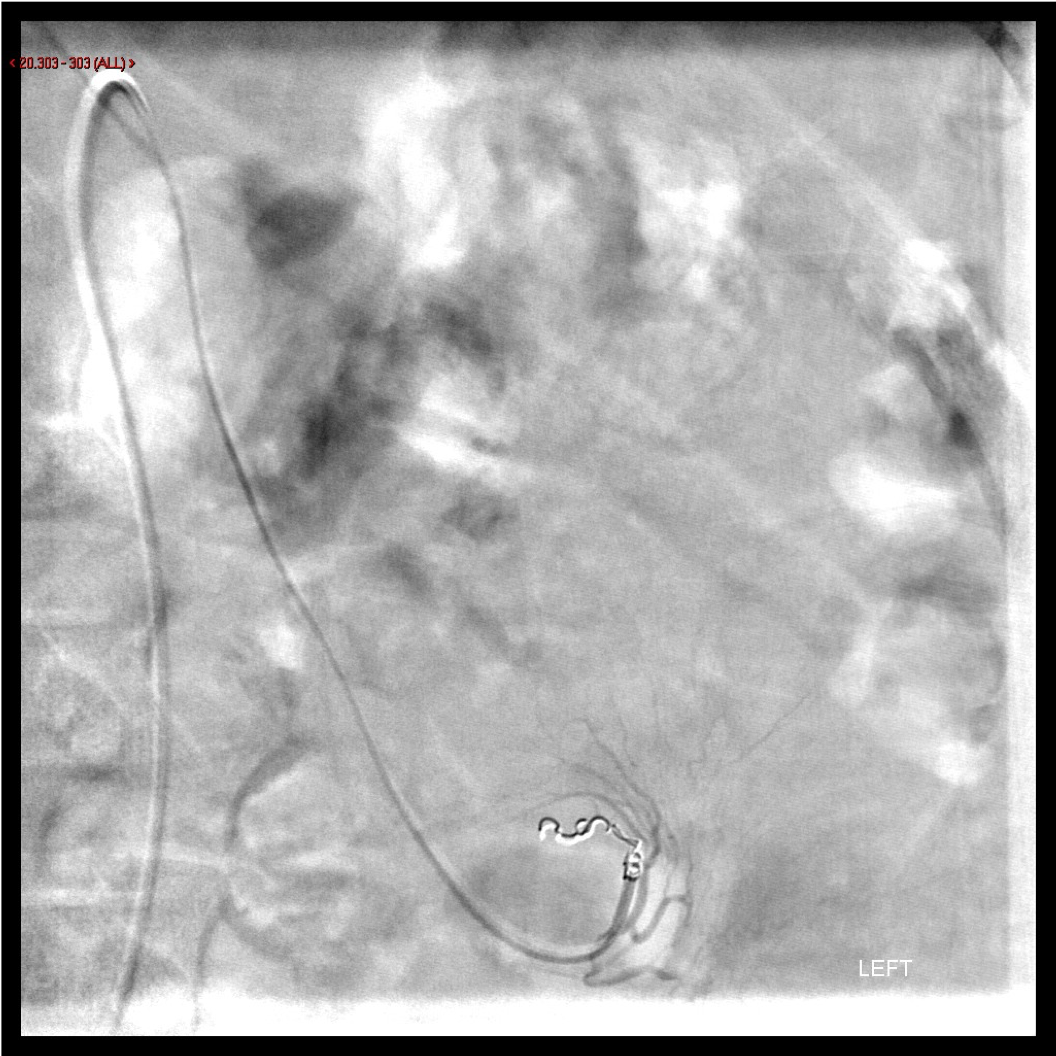
The image to the left depicts a selective arteriogram via the right intercostal bronchial trunk (ICBT). Hyperemia, neovascularity and hypertrophied vasculature are observed in the mid right lung. These are all positive angiographic findings that warrant angiographic treatment in the setting of massive hemoptysis. The catheter pictured is a Mikkelson catheter, which is the classic catheter used to catheterize the ICBT during such procedures.
Question 5:
A selective embolization is performed via the right ICBT. A post-embolization control angiographic image is obtained. What is the relevant finding?
Comparing the pre-embolization image above to the post-embolization image below, we see evidence of interval embolization of the region of hyperemia, neovascularization and hypertrophied vessels. These diseased vessels have been occluded by particles deployed therapeutically by the IR and are no longer perfused by blood. This effectively lowers the patient’s risk for recurrent hemoptysis from these culprit vessels and therefore denote a successful angiographic result.

Angiography
A 35 year-old male motorcyclist presents to the Emergency Room with sharp left knee pain after a motor vehicle collision.
Question 6:
What is the concerning imaging finding?
This lateral radiograph of the left knee demonstrates an anterior dislocation. While knee dislocations are relatively uncommon, they occur most frequently in the setting of high-energy trauma such as motor vehicle collisions. Knee dislocations are described as anterior or posterior based on the displaced position of the tibia relative to the femur.

Question 7:
What additional imaging modality should be requested in light of the imaged finding?
Given the frequent association of neurovascular compromise in the setting of traumatic knee dislocations, *angiographic imaging of the left lower extremity should be performed to assess the status of the arterial outflow and runoff to the leg.
*Note that angiography simply refers to fluoroscopic imaging of the blood vessels or vasculature. Venography and arteriography are more specific terms that refer to fluoroscopic imaging of the veins and arteries, respectively.

Angiography
A diagnostic left lower extremity arteriogram is performed and the following image is obtained.
Question 8:
What is the significance of the depicted finding?
This image shows a diagnostic subtraction left lower extremity arteriogram. Contrast is injected from a catheter in the left common femoral artery and into the left popliteal artery. Here, there is evidence of an abrupt cut off of blood flow in the popliteal artery just above the level of the knee joint. This is secondary to either traumatic dissection (ie. with associated occlusion, preventing antegrade blood flow down the leg) or transection of the popliteal artery (ie. resulting in blood exiting the transected vessel into a rapidly expanding hematoma in the surrounding soft tissues).


Angiography
A 67 year-old male presents from a small community outside hospital with acute onset of bright red blood per rectum. He becomes hemodynamically unstable and a transfer is requested. Given the degree of active bleeding pouring through the colon, Gastroenterology is unable to see the site of bleeding on colonoscopy. Interventional Radiology is consulted for diagnostic mesenteric arteriography to diagnose and treat the source of bleed.
Question 9:
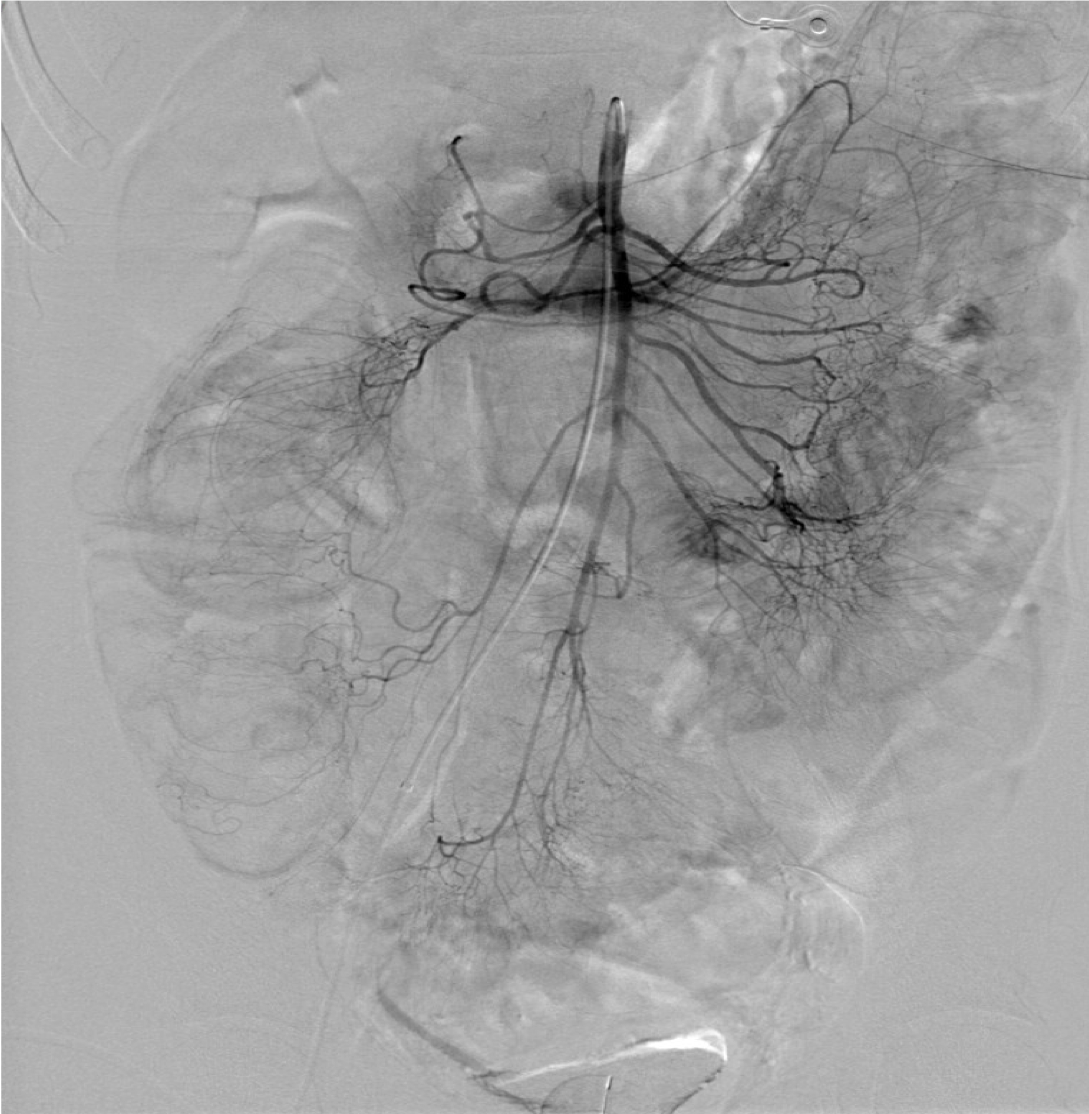
What sort of image is depicted?
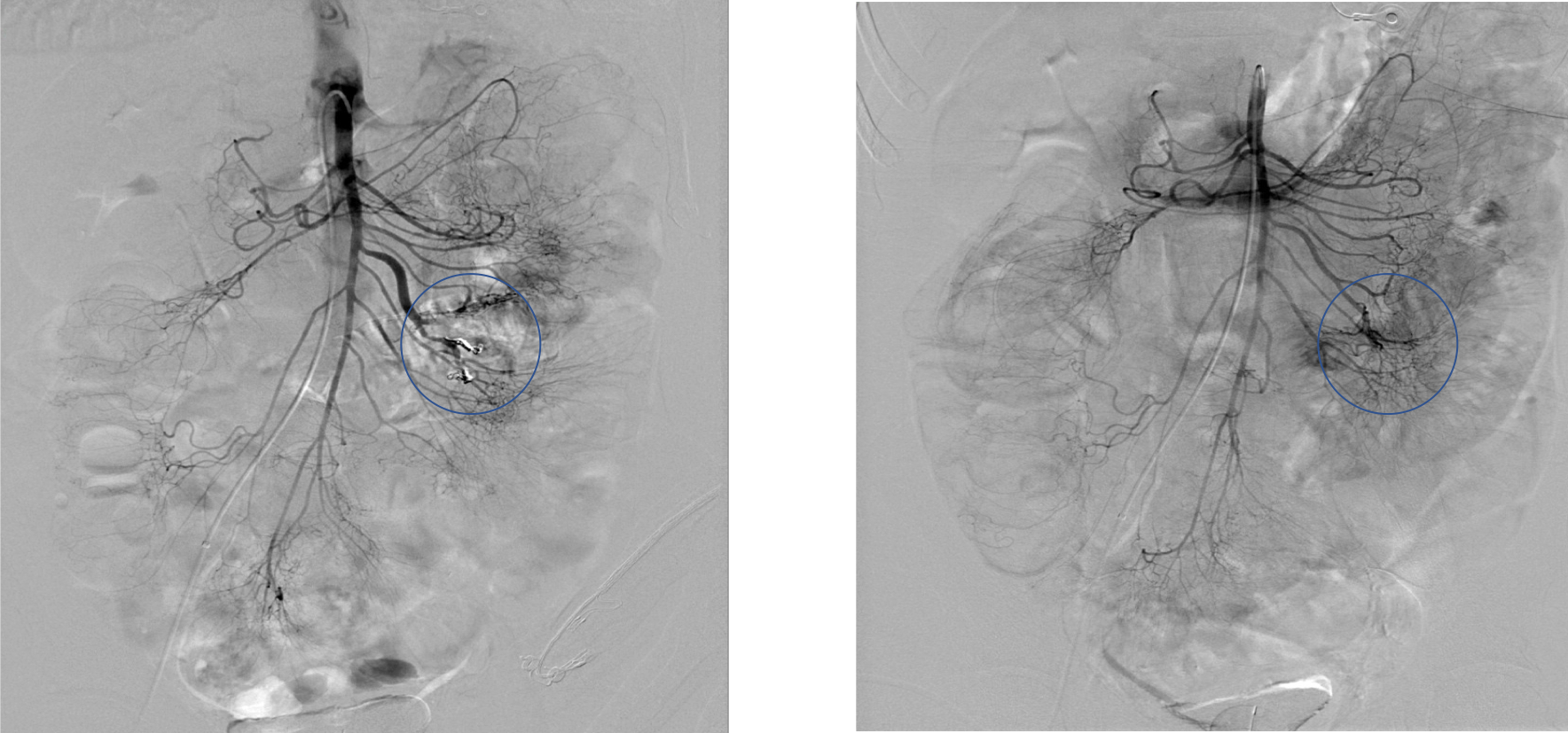
This image is a diagnostic arteriogram using a base catheter who’s tip is parked in the origin of the superior mesenteric artery. This beautiful arteriogram demonstrates the branches of the superior mesenteric artery feeding the midgut (jejunum, ileum and colon to the distal two thirds of the transverse colon).
Question 10:
Is there is a suspicious finding that you feel requires better visualization?
You are concerned about a hazy dark focus of contrast appearing in the region of the branches perfusing the ileum (circled on the image). The IR then uses a microcatheter which she advances coaxially through the base catheter through to the ileal branches perfusing the queried segment of bowel. A selective diagnostic arteriogram is then performed in this region through the microcatheter.


Question 11:
What is the relevant finding?
The circled region reflects a focus of active contrast extravasation. This findings represents angiographic evidence of the source of gastrointestinal bleeding. In addition to active contrast extravasation, other positive angiographic findings that may reflect sources of gastrointestinal bleeding include arteriovenous fistula, or arterial pseudoaneurysms.

Question 12:
What is the next step in management?
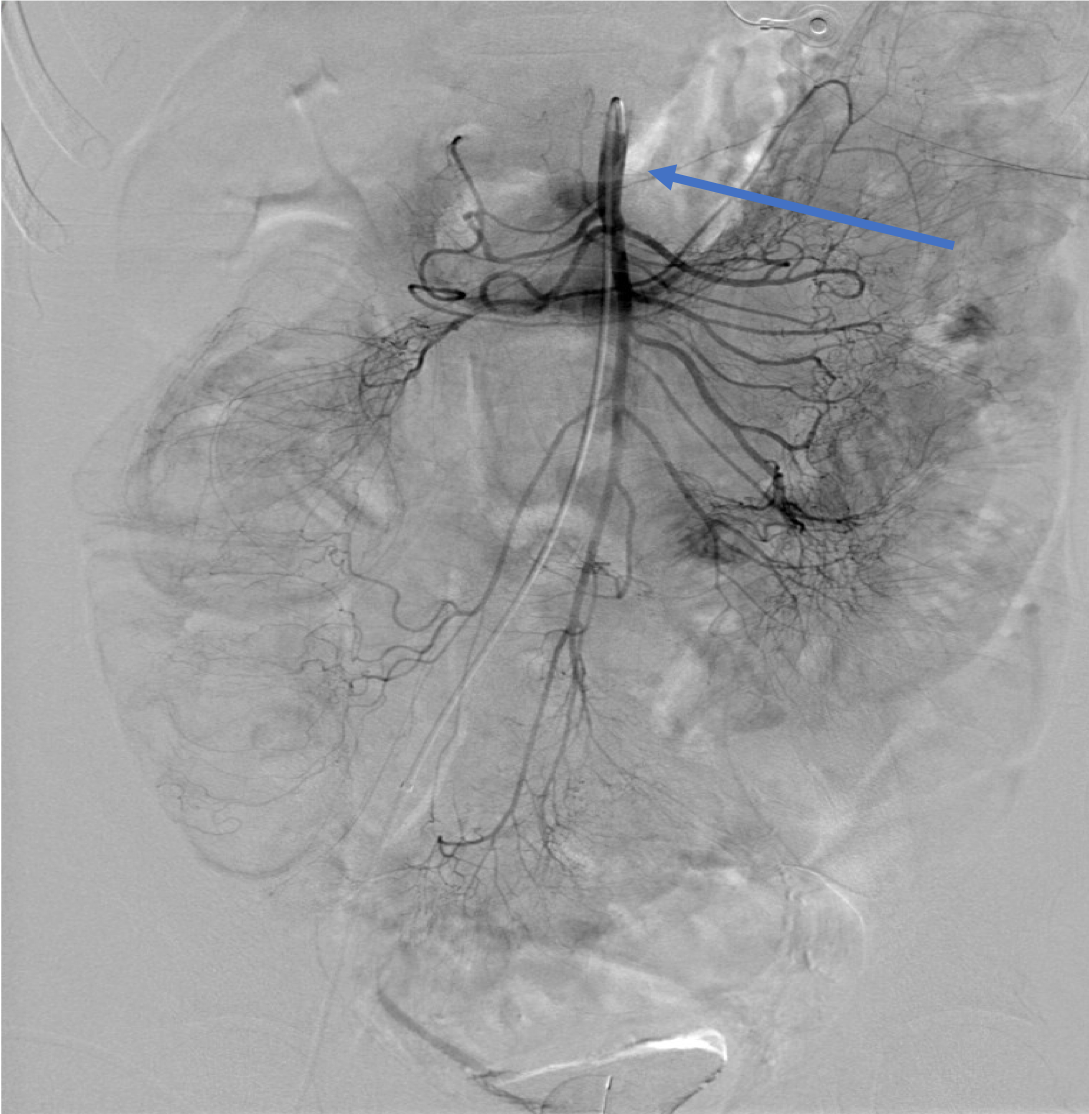
Coil embolization is performed across the arterial arcade feeding the region of active contrast extravasation. Of note, embolizations are performed as distal in the mesenteric vasculature and as close to the source of the bleed as technically feasible, which is typically at the level of the mesenteric arcades. Accomplishing the aforementioned will enable treatment of the culprit bleed while minimizing potential ischemic damage from the therapeutic embolization to an uninvolved, nonbleeding territory of bowel.

Further Explanation:
The images demonstrate the post embolization control diagnostic arteriogram through the superior mesenteric artery (LEFT) and comparative baseline pre-embolization image (RIGHT). Radiopaque coils are noted deployed across the perfusing arcade with evidence of cessation of the previously noted bleeding source.
Angiography
After successful treating the bleeding source, a disk of a nondescript diagnostic study performed of the patient arrives the next day from the tranferring outside hospital. It includes the depicted image.
Question 13:
What sort of study is depicted? What is your next step in management?
The image depicts a positive finding of a focus of bleeding in the ileum in a tagged RBC scan. This radiological (ie. nuclear medicine) study is the most sensitive imaging test designed to assess for gastrointestinal bleeds. A positive finding is a focus of radiotracer uptake that increases in intensity and which moves in the direction of bowel peristalsis. This positive finding corresponds to the site of bleeding treated in the ileal branch of the superior mesenteric artery. You are reassured that the IR treated the sole source of gastrointestinal bleeding in your patient who is now stable.