




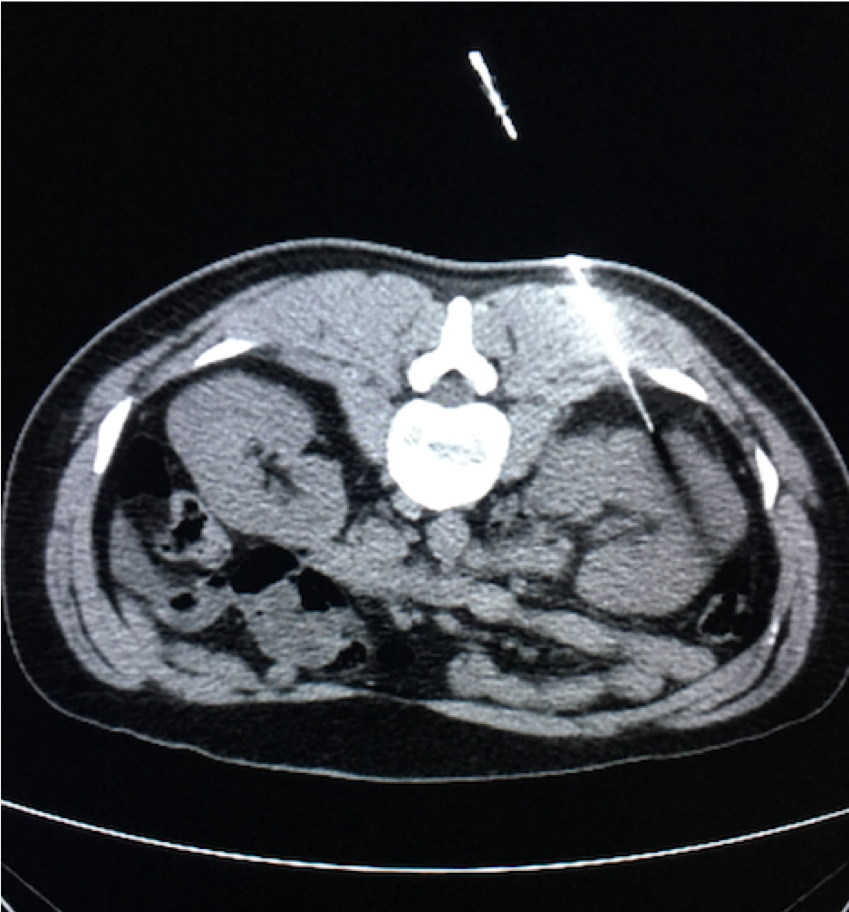
Computed Tomography (CT)
Introductory CT Image
Question 1:
What is the type of imaging modality displayed?
A CT scan without contrast is displayed. The current axial (transverse) slice is made through the patient’s abdomen at the level of the kidneys.
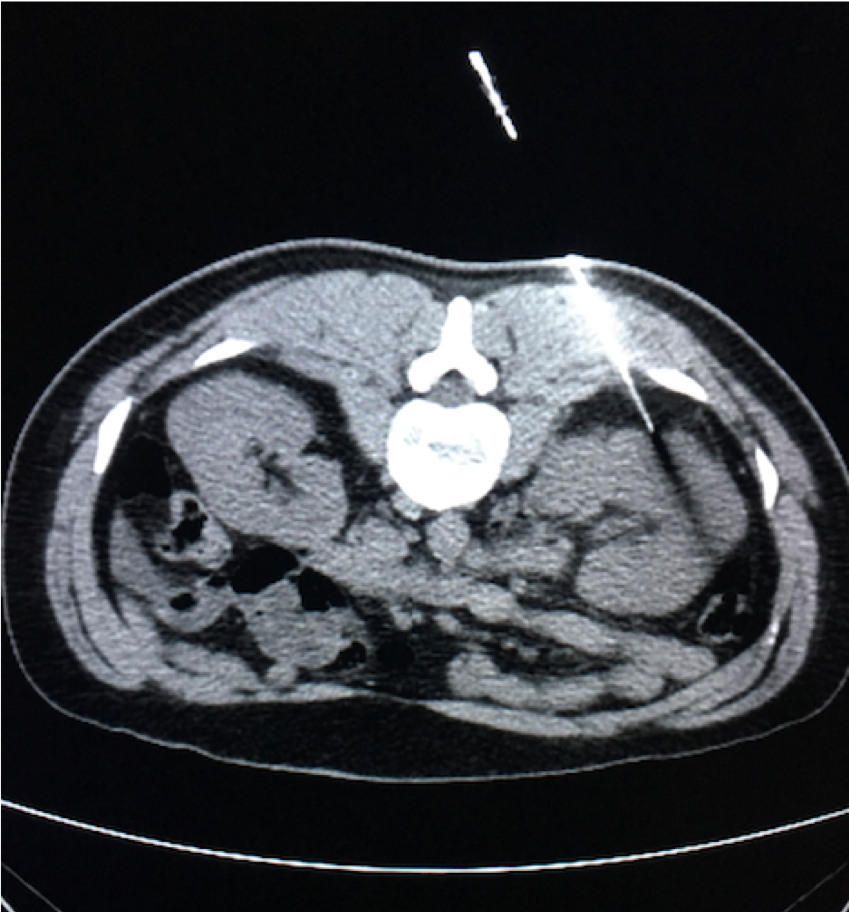
Question 2:
What is this modality being used to perform?
This unenhanced (noncontrast) CT is being used to perform a nontargeted (random) parenchymal biopsy of the kidney in this patient who has proteinuria of unknown etiology. The patient is prone (face-down). A coaxial (i.e. two part system of needle guide and biopsy needle) are advanced into the left kidney via a left paraspinal approach.
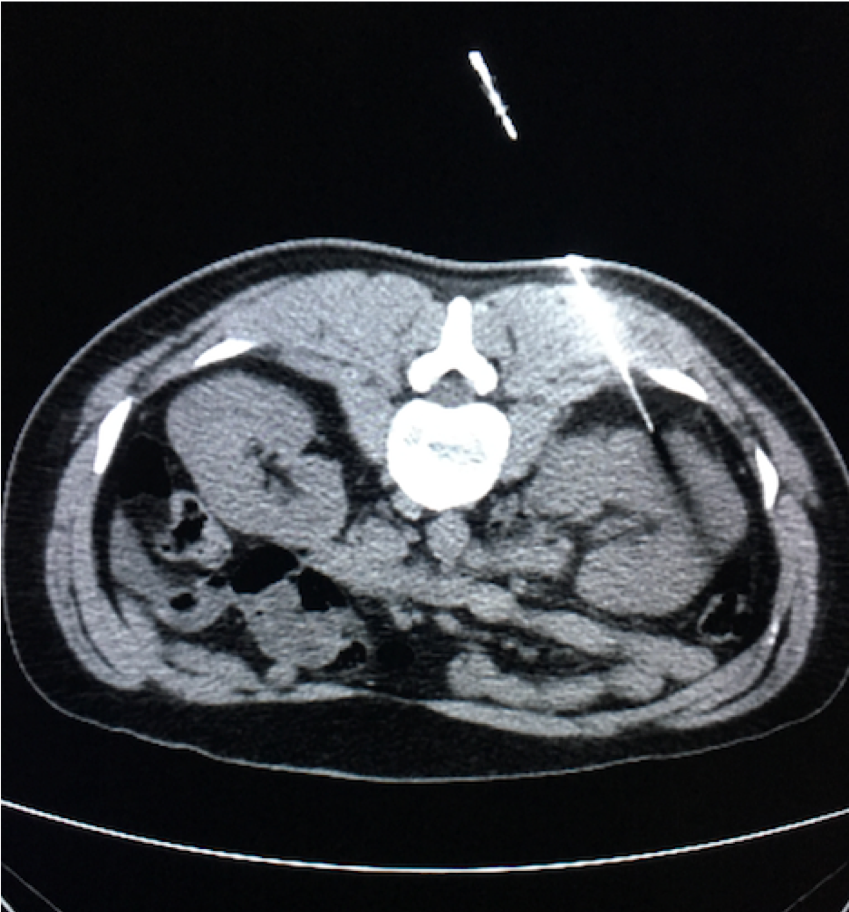
Question 3:
What other modality is often utilized to perform such procedures?
Renal biopsies may be performed under both CT or ultrasound guidance. They are more routinely performed under ultrasound guidance due to the portability of this modality, the absence of associated radiation and the real-time visualization of the biopsy needle as it is advanced into the kidney.
Question 4:
What is the finding of concern in this patient?
A well circumscribed, enhancing solid mass is seen in the kidney. This is a malignant tumor until proven otherwise. The imaging characteristics suggest that a renal cell carcinoma is the most plausible diagnosis.
Question 5:
You learn that this 80 year old patient had her right kidney removed 20 years prior for a large tumor. What is the potential role of the interventional radiologist in managing this patient?
For patient’s who have either life expectancy <10 years, those who are poor surgical risks, with history of previous partial nephrectomy or who have a solitary kidney, percutaneous thermal ablations of renal tumors are considered. While tumors up to 4.5cm can be treated, better results are shown with those <3cm and which are exophytic (partially protruding from the renal parenchyma). This elderly patient with solitary left kidney is a good candidate for a percutaneous thermal ablation by the interventional radiologist.
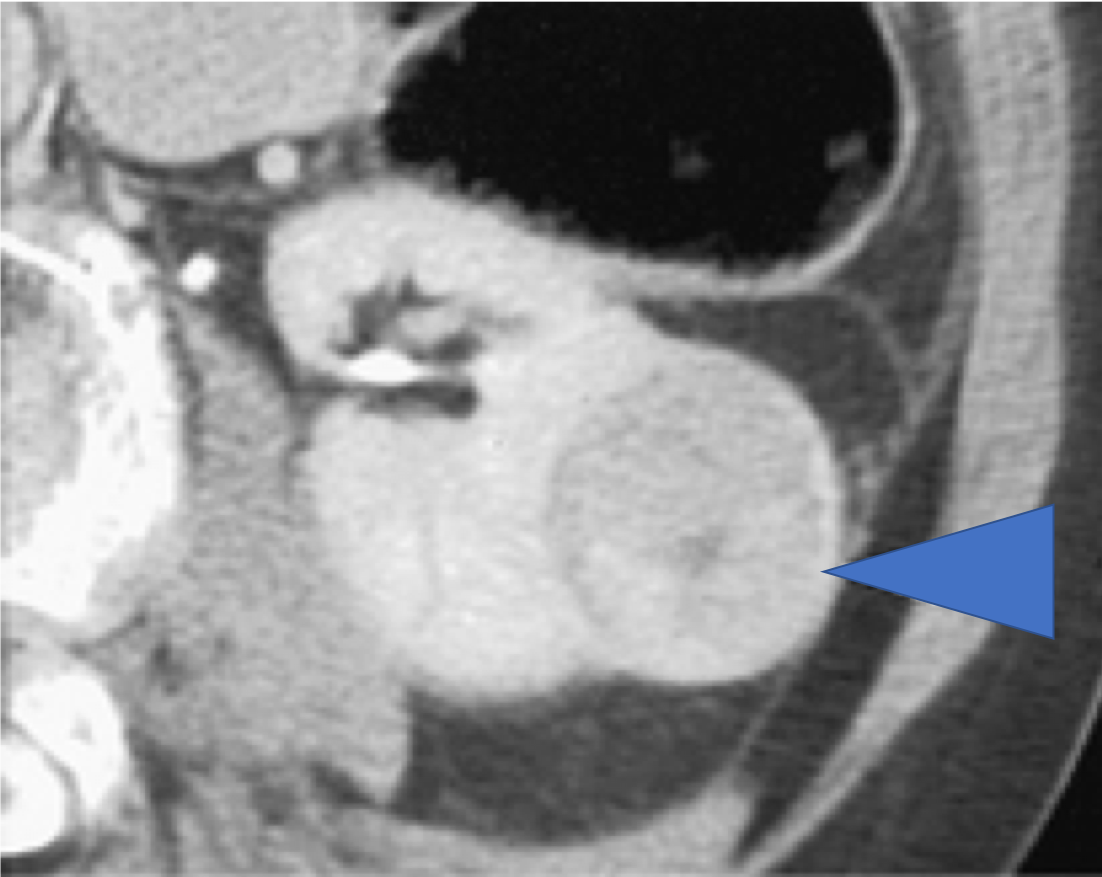
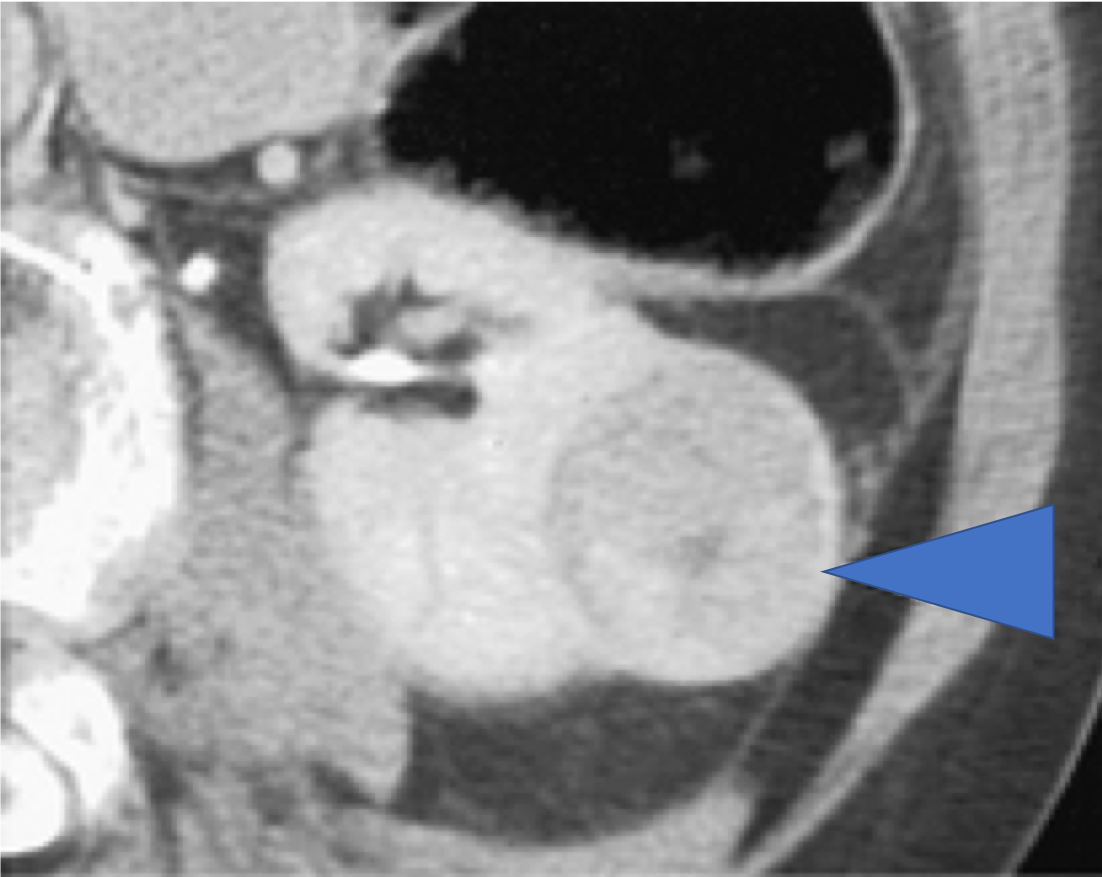
Further Explanation:
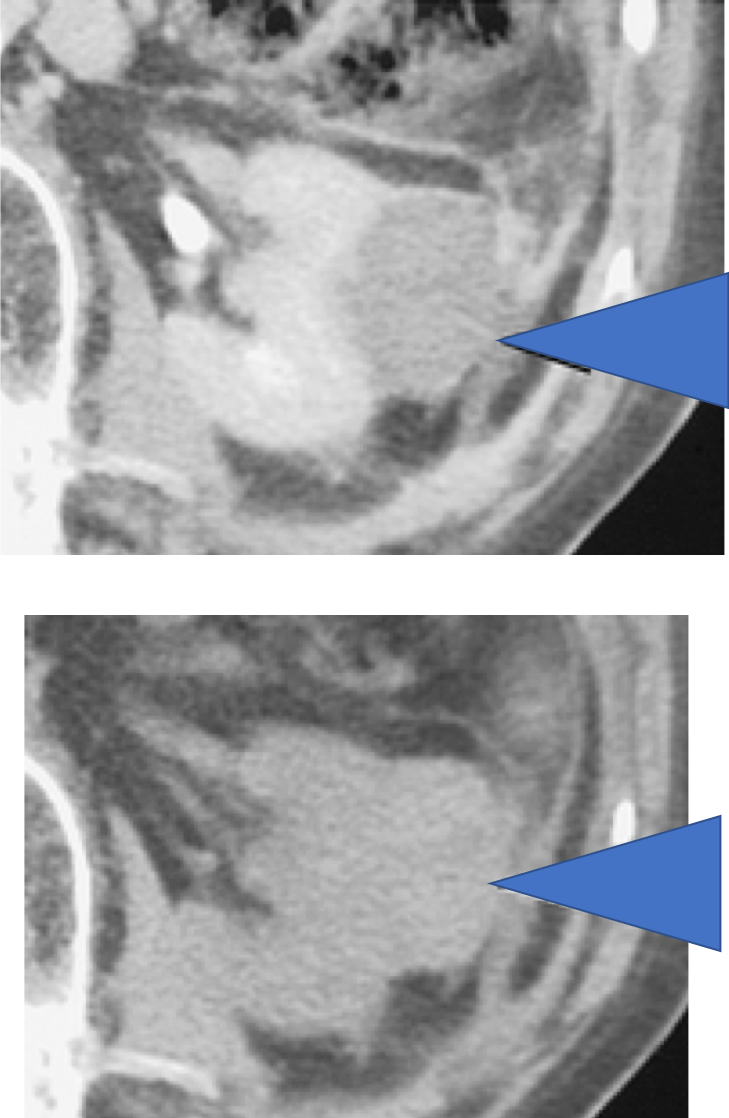
A same session biopsy followed by radiofrequency ablation is performed of the left renal mass by the IR. Biopsy pathology results reveal clear cell renal cell carcinoma. A one month post-ablation CT scan is performed. What are the relevant imaged findings?
Depicted are a contrast-enhanced (above) and an unenhanced image (below) of the ablated renal mass. Note the absence of any contrast enhancement when comparing the two scans. The presence of the noncontrast scan serves as a comparison for the radiologist to ensure that anything that appears hypodense (dark) on the noncontrast scan remains hypoenhancing (dark, given failure to retain contrast) on the contrast-enhanced scan. Such findings ensure that the radiologist correctly assesses the treated mass for absence of residual or recurrent viable tumor (ie. the desired outcome). The images suggest that there is no enhancing or viable residual tumor, connoting a successful ablation of this patient’s renal cell carcinoma.
Question 6:
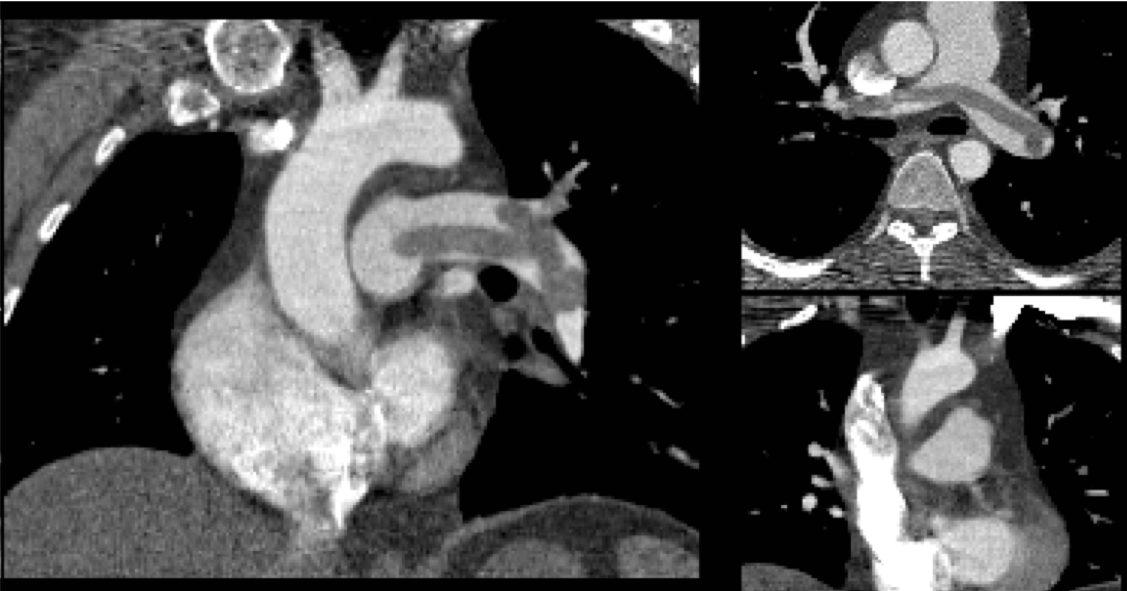
A 56 year old male truck driver with a history of hypertension, presents with acute onset shortness of breath and tachycardia after a long trip across the eastern seaboard. A CT angiography of the chest with attention to the pulmonary arteries is obtained by the emergency room provider. What are the pertinent findings?
The CTPA demonstrates a ”saddle pulmonary embolus” . This is a large burden of thrombus which is splayed across the right and left pulmonary arteries and usually heralds an imminent hemodynamic insult. In the setting of pulmonary embolism, particularly saddle PE’s, a pertinent finding to assess for is cardiac strain, evidenced by straightening or in severe cases leftward bowing of the interventricular cardiac septum. Cardiac strain is a poor prognostic factor of a PE.
Question 7:
The patient becomes hypotensive and is found to have a troponin leak. The patient is started on intravenous anticoagulation. A decision is made to administer 100 mg of alteplase (rt-PA) intravenously over 2 hours. After slight improvement in hemodynamics, 2 hours later the patient become unstable. What is the possible role of the interventional radiologist?
The American College of Chest Physicians (ACCP) defines acute massive PE as PE with hypotension (SBP <90mmHg for >15 minutes b. hypotension requiring vasopressors or c. clear evidence of shock. In such settings, Thrombolytic therapy (systemic rt-PA administered via a peripheral IV) is the first option for pulmonary embolism with hypotension (Grade 2B recommendations). If systemic thrombolysis therapy fails or is contraindicated, catheter-directed therapy by the interventional radiologist is regarded as the treatment of choice.
Further Explanation:
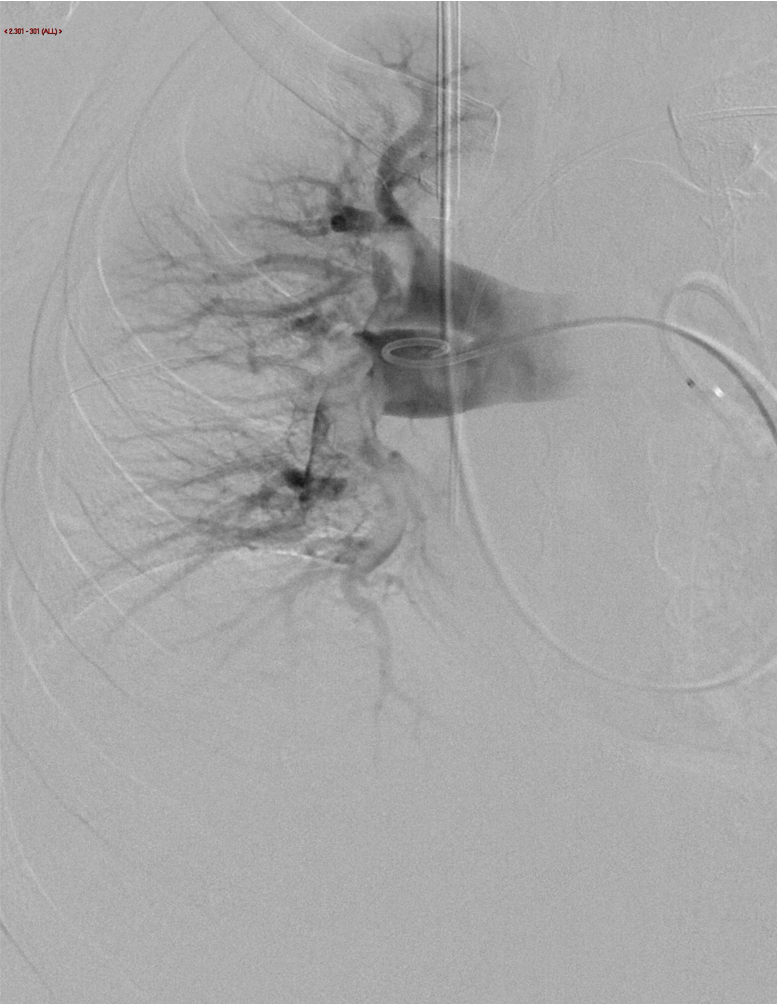
Interventional Radiology is consulted for catheter-directed thrombolysis. What are the indications for catheter-directed thrombolysis (CDT)? How is it utilized?
CDT is thought to be a potential lifesaving therapy in massive PE patients with hemodynamic shock who have:
A. failed response to systemic thrombolysis
B. inability to tolerate systemic thrombolysis
C. unavailable or contraindicated surgical embolectomy
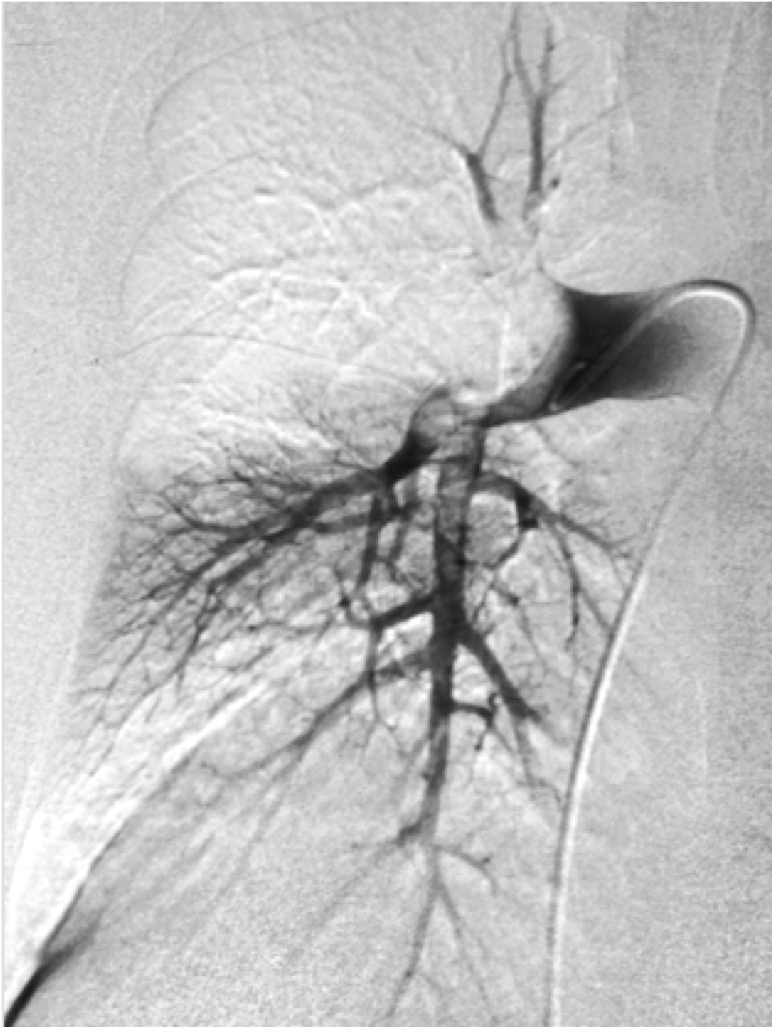
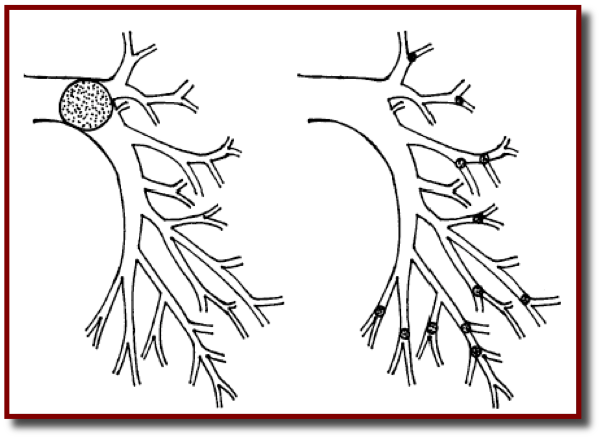
It was originally inspired by experience with CDT of peripheral bypass grafts and dialysis fistulas, and was developed supported by superior results from animal models of PE employing direct intrathrombus drug delivery. When a thrombolytic is utilized, it requires a dosing that is 10-20% of that used in systemic thrombolysis therapy. The image to the left is a digital subtraction angiographic image performed during right pulmonary arterial angiography through a pigtail catheter advanced from the right internal jugular vein into the right pulmonary artery via the SVC. Evidence of filing defects in the lobar, segmental and subsegmental right pulmonary artery branches represent thromboemboli (“embolized thrombus”).
Question 8:
What are the mechanisms by which catheter-directed therapy (CDT) performed by the IR improves oxygenation in patients suffering from pulmonary emboli?
The goals of CDT are the following:
1. Increase the luminal cross-sectional area of the pulmonary artery that is perfused with blood: The techniques used by the IR to accomplish this are Aspiration thrombectomy and Stent recanalization.
2. Increase the surface area of clot that is available for lysis (either by intrinsic mechanisms of thrombolysis, a la ”autolysis” or by any administered thrombolytic such as rt-PA): The techniques used to accomplish this are fragmentation thrombectomy and rheolytic thrombectomy.