




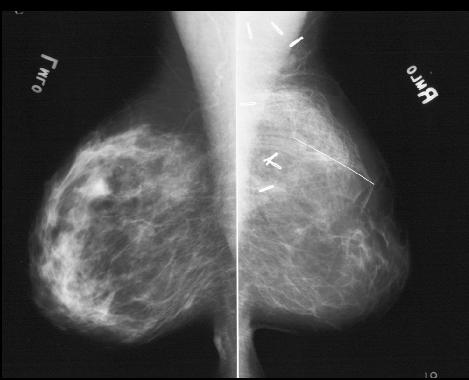
Case 1
45 year old female with history of partial mastectomy and breast reconstruction
Question 1:
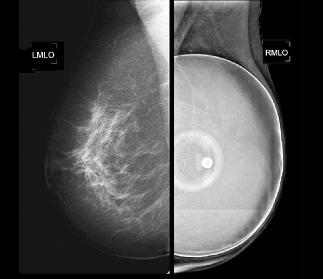
a) What is this study called?
This is a mammogram
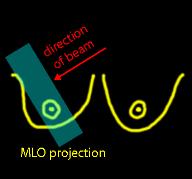
b) What is this view called?
These are MLO views, meaning medio-lateral oblique (see labels saying LMLO and RMLO)
c) Which is the reconstructed side?
Look for surgical clips as a clue.
Case 1
The link below will bring up a diagram to illustrate how an MLO view is obtained. By convention, most radiographic projections are described with reference to the path of the x-ray beam through the patient. So an MLO view means the beam went from medial to lateral to receptor.
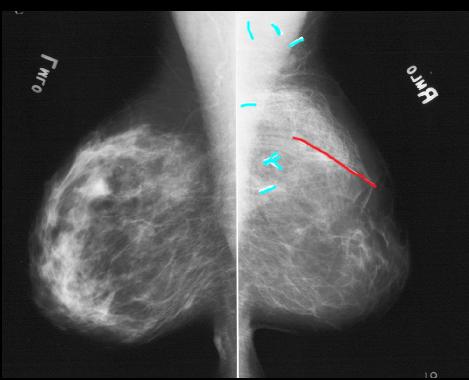
Question 2:
a) What is indicated below in red?
This is actually not inside the patient, but is a type of marker placed on the skin by the mammography technologist, to mark a scar.
b) Why do we typically display mammogram images back-to-back?
This is because, while different patients may have very different appearances of their breast tissue on mammograms, most patients are very symmetric from side to side, and displaying the images in this way helps us to pick up subtle differences that may indicate disease.
c) Other than the clips and marker, do you think this patient's two breasts look symmetric?
NO! The left breast show a more natural appearing distribution of dense stroma extending out in a branching pattern from the region of the nipple. The pattern in the right breast is very different, with not much tissue behind the nipple and an odd swirling pattern in the upper part of the breast, where the surgical clips and scar marker are located.
Case 1
This is a different patient who also has a surgical history.
Question 3:
a) What surgery did this patient have?
There is an artificial object in their right breast, an implant. There is almost no breast tissue over the implant, just skin, so they likely had a mastectomy (complete breast removal), with reconstruction using an implant.
b) What are two types of implants that may be used for breast reconstruction?
The implant may be filled with saline (as this one is, because you can see the internal components and port for filling the implant), or with silicone (which is denser than water and shows up as very white on a mammogram, with no visible internal structure that can be seen).
Case 1
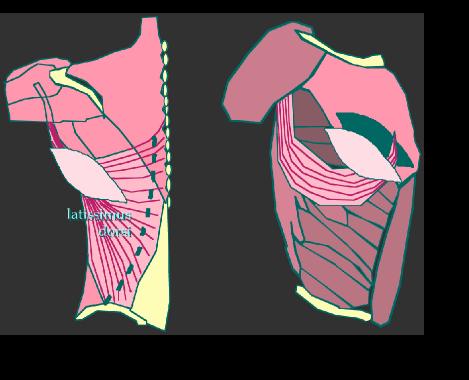
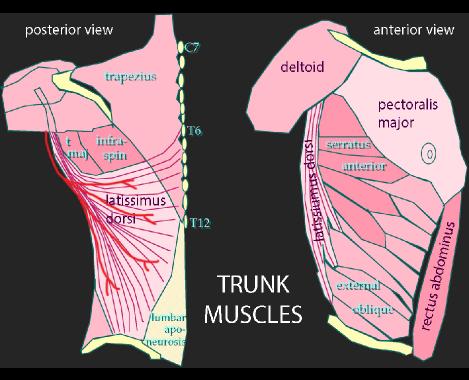
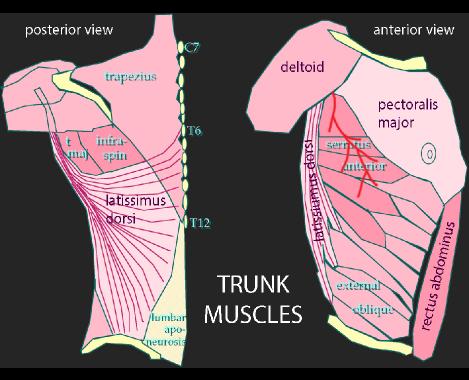
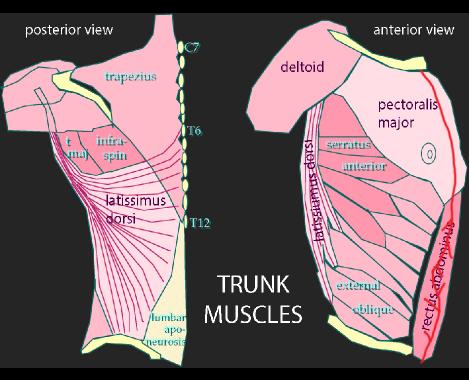
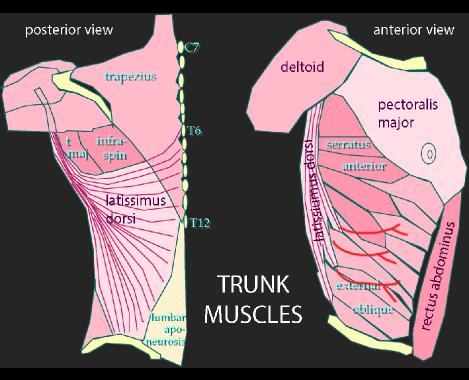
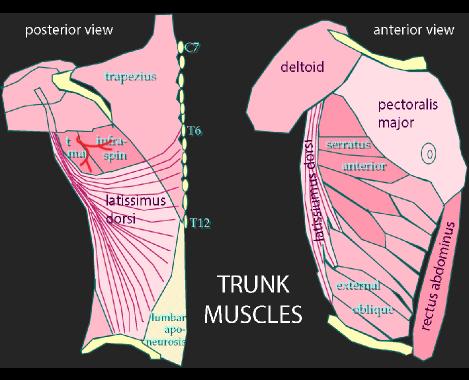
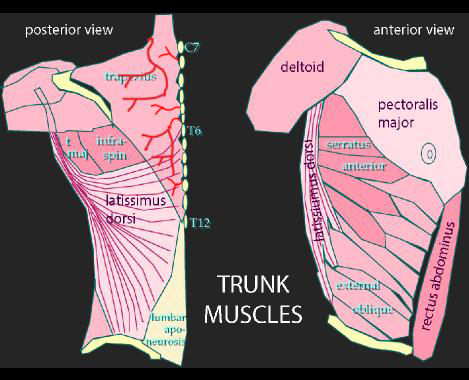
This diagram provides a review of the chest wall and upper abdominal muscles, with focus on their blood supply.
Question 4:
a) Why is knowledge of the blood supply of these muscles important in our patient's case?
Our patient had a reconstruction of a part of their breast (after partial mastectomy or lumpectomy) using her own body musculature. In order to select an appropriate muscle to do a reconstruction (either a flap or a free flap), it is important to understand where the blood vessels are located and whether it will be easy to find and preserve them.
b) After reviewing the blood supply shown below, which muscles would be easiest to move into the region of breast surgery for reconstruction while maintaining their native blood supply?
The two muscles that are easiest to move into the upper anterior chest are the latissimus dorsi (keeping its blood vessel, the thoracodorsal artery, intact while swinging the muscle around), and the rectus abdominus (which has blood supply from above via the superior epigastric, as well as from below via the inferior epigastric).

Case 1
This diagram shows how a latissimus flap is done. A portion of the muscle with its blood supply is cut free, and any overlying subcutaneous fat (and skin if needed) are moved around to the anterior chest wall.
Question 5:
Which approach will provide a larger volume of tissue for breast reconstruction: latissimus flap or rectus flap?
Usually there is more overlying fat in the lower abdomen that can be brought up into the anterior chest with a rectus flap than there is with a latissimus flap. Because our patient had only a partial mastectomy, a latissimus flap was sufficient to provide a good cosmetic result.