




Case 4
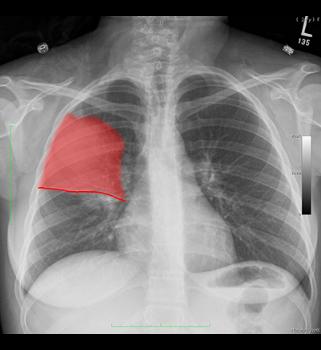
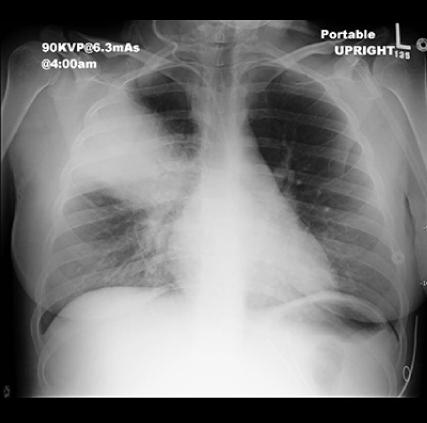
This is a 23 year old female with cough and high fever for the past three days, feeling worse and more short of breath.
Question 1:
a) Given her history, what is the most likely diagnosis?
This sounds like a community-acquired pneumonia.
b) Given her chest radiograph, what is the most likely etiology?
This appears to be a lobar consolidation, so pneumococcal pneumonia is most likely.

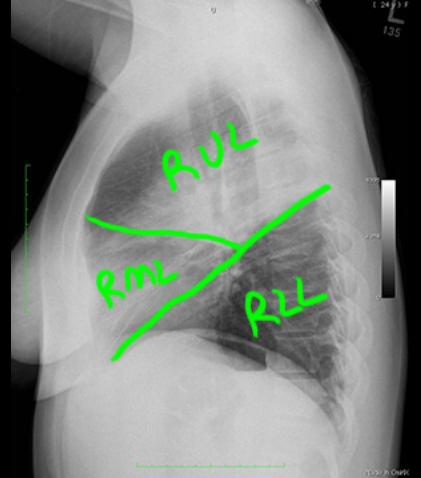
Case 4
This is the patient's lateral chest radiograph.
Question 2:
a) How would you describe the abnormality on this view
This is a hazy opacity, consistent with an airspace filling process such as pneumonia.
b) What lobe is involved?
The opacity has a sharp horizontal inferior border suggesting that it is abutting a fissure. This is consistent with location within the right upper lobe.

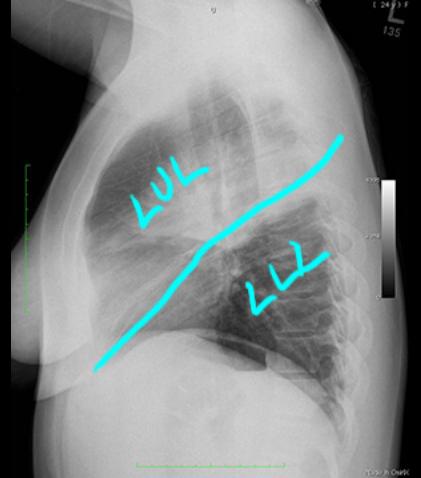
Case 4
This is the same lateral view, with structures outlined by clicking the links below.
Question 3:
What is indicated in green and purple on the annotated image showing fissures?
Green is the minor fissure (horizontal fissure). Purple is the major fissure (oblique fissure).


Case 4
This is a followup image on our patient, who continued to be febrile despite antibiotics and here blood pressure was beginning to drop. It was decided on insert a central line (CVL-central venous line) to administer stronger antibiotics.
Question 4:
a) What is the significance of a drop in blood pressure in this patient?
This is worrisome for sepsis, and warrants more aggressive treatment of her pneumonia.
b) What is the commonest approach for insertion of a CVL (central venous line)?
The right internal jugular vein is the commonest approach, as the path to the superior vena cava is the most straight.
c) What approach was used in this case?
The CVL seems to be coming down from the right side of the neck toward the mediastinum, so a right IJ approach was likely chosen.
Case 4
After placement of the CVL, the patient did not improve, and in fact, nurses noted that they were having difficulty with the IV medications, as they did not seem to flow into the catheter very well.
Question 5:
a) There is another new support line present on this image. What is it?
An endotracheal tube has been inserted.
b) Does the pneumonia look like it is improving?
No, the area of consolidation in the right lung looks more extensive.

Case 4
The labels below show other changes that can be seen on this image.
Question 6:
a) What is the significance of a widened mediastinum?
Given that the CVL does not seem to be working well, this should raise the concern of bleeding into the mediastinum and possible malposition of the catheter.
b) Is the endotracheal tube in satisfactory position?
Yes, its tip is below the thoracic inlet and not near the carina, so it seems to be in good position.
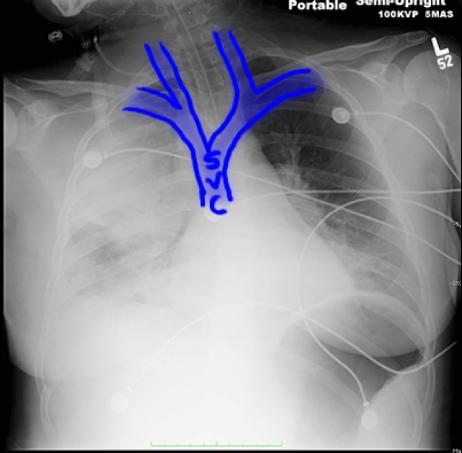
c) Pertinent veins of the mediastinum are shown below. What two veins come together to form the SVC (superior vena cava)?
The right and left brachiocephalic veins form the SVC.


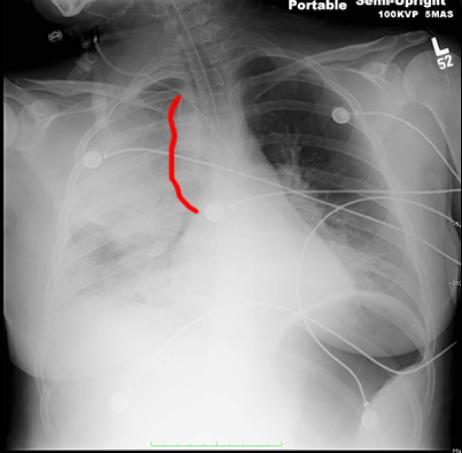
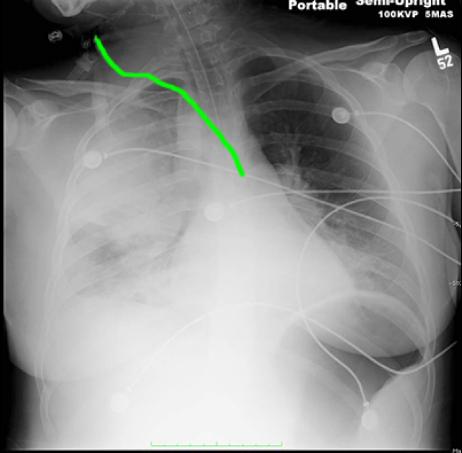
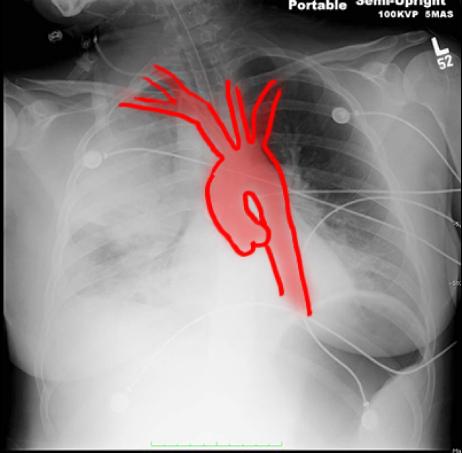
Case 4
This is the same portable chest radiograph on our patient.
Question 7:
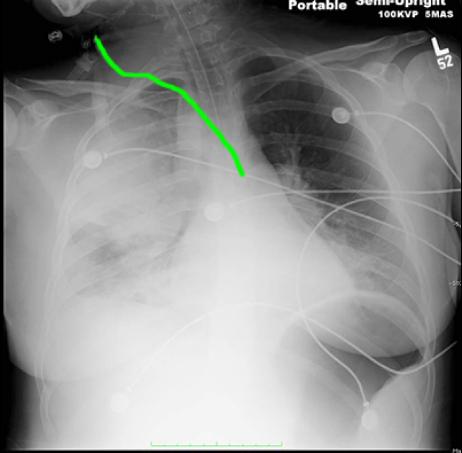
a) Is the course of the CVL normal?
No. Based on the prior images outlining the veins of the mediastinum, the CVL is passing too far to the left to be in the right brachiocephalic vein and superior vena cava (SVC).
b) What vessel might the CVL be in?
If you look at the arteries shown below, the course of the CVL suggests that it may be in the carotid artery instead of the internal jugular vein.
c) What patient history is most consistent with inadvertent arterial placement of a CVL?
This most often happens in patients with very low blood pressure, as our patient was experiencing due to sepsis. In that setting, arterial and venous blood can look very similar, and this may compromise accurate CVL placement.