




Case 1
This 41 year old male has vague right thigh pain and swelling. He is not sure when it started but it has been going on for at least several months.
Question 1:
a) What is this study?
This is a radiograph of the thigh/femur. It would routinely be done in the AP projection in the supine position. Recall that the chest is the only part of the body that we routinely do frontal imaging in the PA projection (to minimize magnification of the heart). Some limb radiographs are done in the standing (upright) position but only if specifically requested. This is most often done to evaluate effects of load on joints like the hip, knee and joints of the foot.
b) What different densities can you identify on this study?
Since it is a radiograph, our ability to discriminate slight differences in tissue density is not as good as for CT, since we are viewing a summation of all the different tissues the beam passed through. We can see metal (in a gonadal shield), calcium (of varying density in different parts of the bones), soft tissue (which makes up most of the rest of the limb), air (outside the body) and fat (if there is enough of it present, with optimal orientation relative to the direction of the x-ray beam). Fat and soft tissue are very similar in appearance and can be hard to tell apart on a radiograph.

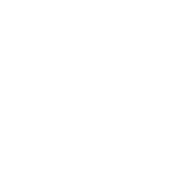
Case 1
This is the same image, with some of the structures outlined using links below.
Question 2:
a) What are the different parts of the femur (indicated on the label below) called?
The magenta/purple area is the diaphysis (the central tubular part of a long bone like the femur), the red area is the metaphysis (the part of the bone that flares out near the end), and the yellow area is the epiphysis (the expanded end of a bone where it articulates with other bones).
b) What is labeled 'mystery3' below?
There is an oval area that appears lower in density than the other surrounding soft tissues, indicated by the label below. It is centered on the diaphysis (shaft) of the femur.
c) Where is the region labeled 'mystery3' located with respect to the femur?
It is not possible from this single image to tell if the abnormality is anterior, surrounding, or posterior to the femur. You need a lateral view to answer this question.





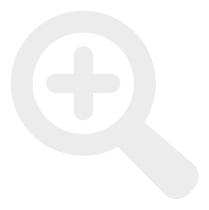
Case 1
This is a labeled view of the patient's AP femur radiograph.
Question 3:
a) What is located at the red dotted line on this image?
There is often a faint transverse line visible in adults at the point where the metaphysis meets the epiphysis. This marks a scar where the growth plate closed at the end of puberty. The growth plate (physis) is a cartilaginous zone between the epiphysis and the metaphysis where elongation and remodeling of the bone takes place during growth. Once growth is completed (at the end of puberty), the cartilaginous zone closes and becomes incorporated into the adjacent bone.
b) What are examples of some specific tissues that make up 'soft tissue'?
Soft tissue density on a radiograph includes such elements as muscle, fascia, lymph nodes, organs, blood, tumors, water, and cartilage. Some of these can be separated on CT images (using the appropriate windows) but they cannot be identified separately on radiographs because they are too similar, and also because of the summation of many different tissues on the final image, which limits the ability to discriminate very subtle differences in density.

Case 1
This is another image on the same patient.
Question 4:
a) What is this image?
This is a lateral view of the thigh/femur. Again, this is generally done in the supine position, but can be done standing if desired.
b) Can you see the abnormality that was visible on the AP view? Where is it located relative to the diaphysis (shaft) of the femur?
The oval fatty density is faintly seen anterior to the femoral diaphysis. It is bowing the adjacent muscles anteriorly. If you look closely at the anterior skin and subcutaneous fat, you can see that they are bowed forward slightly by this palpable mass.

Case 1
This is the same lateral view, with findings marked below.
Question 5:
a) If you bring up the mystery outline below, why does the inferior part of the lesion look more lucent than the superior part?
This is probably due to overlap between the lesion and large muscle bundles of the quadriceps that lie lateral or medial to it. Again, the final density seen on the projection radiographic image is a sum of all the tissues encountered by each part of the beam.
b) Is the density of the lesion the same as the density of the subcutaneous fat?
The subcutaneous fat looks slightly more lucent than the lesion, but this is again likely affected by overlap with other tissues. In this projection, the subcutaneous fat is not summated with any other tissues except a thin layer of dermis, so it is almost pure fat density. The lesion is likely at least partly overlapping with muscle groups as well a skin, which will alter its apparent density on the image. To get an accurate reflection of its density, you would need to do a cross-sectional study, like CT.


Case 1
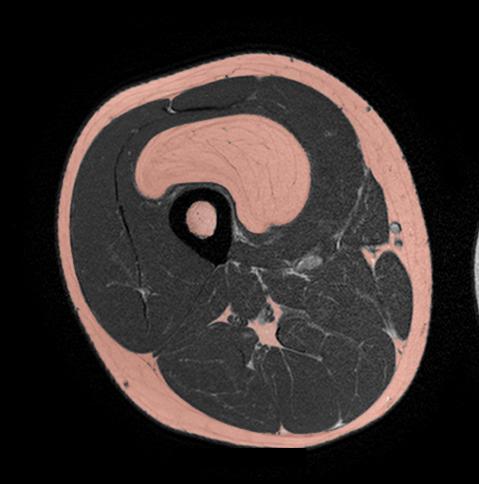
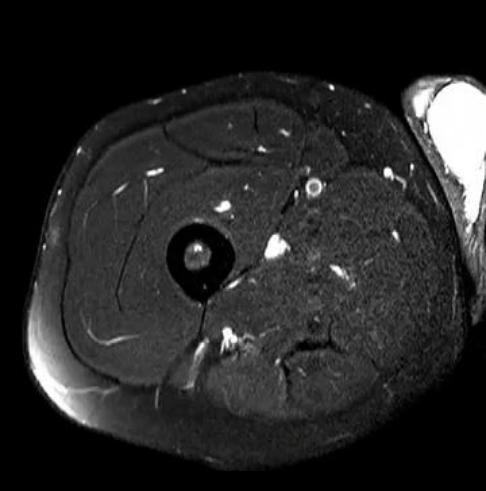
This is another imaging study on the same patient.
Question 6:
a) What type of study is this?
This is an MRI--cortical bone is very dark. There is no fat suppression, so fat is bright. No high signal is seen in the region of the synovial space of the knee, so this is T1-weighted imaging (fluid is dark, and any joint fluid is inapparent since its signal is close to that of adjacent bone or ligaments).
b) Try to find the lesion we have seen on the radiograph. Is it low density on this image?
The lesion is anterior to the femur, wrapping from anteriorly to the medial part of the thigh. MRI has nothing to do with density, so it does not make sense to call something 'low density' on an MRI image. We talk instead about 'signal'. The lesion has high signal, similar to that of subcutaneous fat. This suggests that it is composed of fat, since fat is the only bright tissue on this sequence.
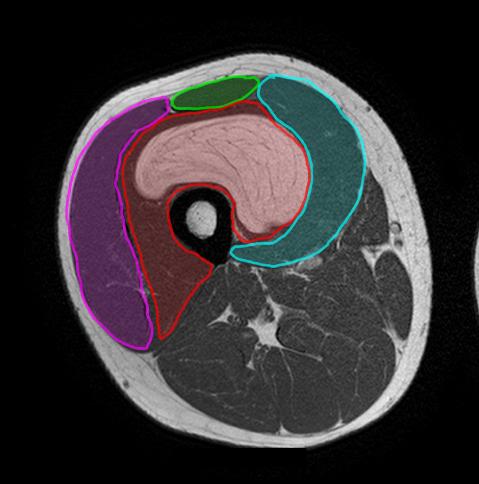
Case 1
This is a selected image from the previous MR series, with structures labeled below. Try to identify the various anatomic structures before clicking the labels.
Question 7:
a) What are the individual muscles that make up the quadriceps femoris?
The four components of the quadriceps femoris are labeled below: green for rectus femoris, blue for vastus medalis, red for vastus intermedius (which contains the fatty lesion), and purple for vastus lateralis.
b) What are the muscles in the thigh adductor group seen on this slice?
Three muscles are outlined below: yellow for sartorius, orange for gracilus and light green for adductor magnus.
c) What are the muscles of the hamstring group seen on this slice?
The short head of the biceps femoris is shown in pink, the long head in brown, semitendinosus in blue and semimembranosis in purple.


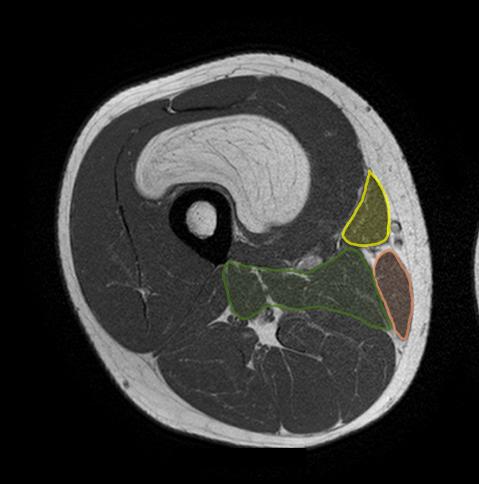

Case 1
This is the same MR slice, with a label indicating neurovascular structures for you to identify.
Question 8:
What neuromuscular structures are labeled below?
Dark blue is the greater saphenous vein (medial in location); red is the femoral vessels and femoral nerve, within the adductor canal; light blue is the deep femoral vessels and green is the sciatic nerve.

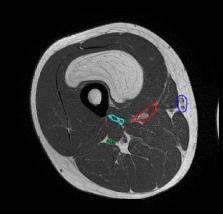
Case 1
This is more imaging on the same patient.
Question 9:
a) What is this study?
This is an axial MR sequence (cortical bone remains dark), with fat suppression (fat is now dark, similar to CT), and T2 weighting (fluid is bright). The vessels are also bright, so 'bright blood' technique has been used.
b) Was IV contrast given for this imaging sequence?
IV contrast is sometimes used for MR, but it is based on gadolinium, which has magnetic properties. This is very different from the IV contrast that is used for CT, which is based on iodine (very dense). However, no gadolinium was used for this T2-weighted sequence because gadolinium only has effects on T1, and is only used for T1-weighted sequences, where it will make vessels look bright. The brightness of the vessels in these images was obtained in a different way, by adjusting the way the scan parameters were set up. You can choose to make vessels look dark or bright, depending on the particular sequence you use.
Case 1
This is a selected image from the previous MR sequence.
Question 10:
a) What is seen medial to the thigh on this image?
There is fluid in the scrotum, which is very bright. This is called a hydrocele, and is relatively common, particularly after injury or infection. Most resolve on their own over time, but if they are large, they can be drained. This one is fairly small and would likely not require treatment.
b) Why might a sequence like this be useful in our particular case?
Fat suppression can be used to make areas of abnormal fluid stand out. But fat suppression also confirms our initial theory that the mass in this patient was made of fat. If you review the entire sequence, the mass went from bright on T1-weighted imaging to dark on T2 with fat suppression, similar to the pattern seen in the patient's subcutaneous fat. This indicates that this lesion is likely composed of fat, and is most likely a lipoma, a common benign fatty growth but most often seen in the subcutaneous tissues. If a presumed lipoma is causing symptoms, it may be removed. In some cases, an apparent lipoma may actually be a well-differentiated liposarcoma or malignancy of fatty cells. This is another reason to remove them, particularly if they are in an unusual location such as this case, to be sure of the diagnosis.
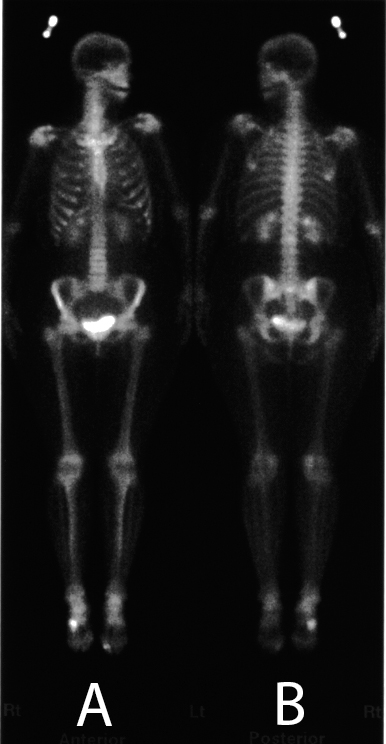
Case 1
This is a different patient with foot pain, and a recent diagnosis of lung cancer. He had this study as part of his staging workup. The patient had developed new pain in his right foot.
Question 11:
a) What is this study and how does it differ from other types of radiologic imaging?
This is a bone scan, a type of nuclear medicine imaging. In nuclear medicine studies, a radioactive tracer is administered to the patient and emitted radiation from the body is collected to generate an image of the distribution of the tracer. Nuclear medicine imaging is the only type of radiologic imaging that uses radioactive agents that emit radiation within the patient's body. The different agents are designed to home in on different tissues or physiologic processes. So it is sometimes also called 'functional imaging'. In the case of a bone scan, it shows where bones are undergoing turnover.
b) What parts of normal bones are most evident on these images and how does image A differ from image B?
The highest activity in normal bones is seen near joints, since this is where bone is always undergoing turnover, due to stresses of normal activity. Because the radiation is coming from within the patient's body, the detector must be brought close to one side of the body to generate the image. In image A, the detector was closest to the anterior part of the body, so structures like the patella and sternum are seen best. In image B, the detector was brought closest to the posterior part of the body, so this image shows the spine and ischial bones more clearly
c) What are mysteries 1 and 2 below?
Mystery1 outlines the kidneys and bladder. As you could imagine from this appearance, the tracer used in bone scanning is excreted by the kidneys. It is normal to see them lighting up like this. Mystery2 corresponds to where the patient was having pain. This is not a normal appearance. Increased uptake like this can be due to anything that increases bone turnover, which could include trauma/healing fracture, infection, arthritis, or tumor.

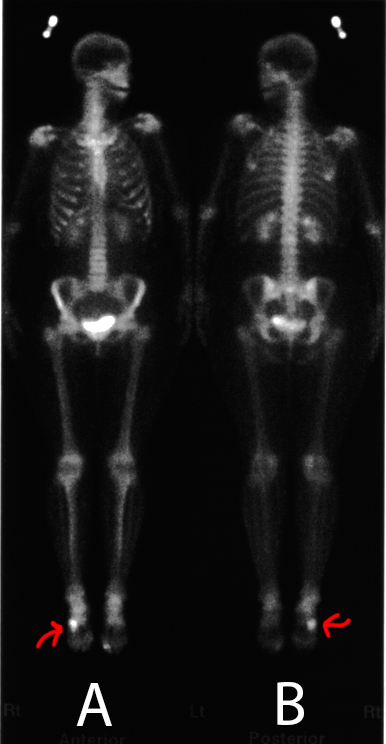
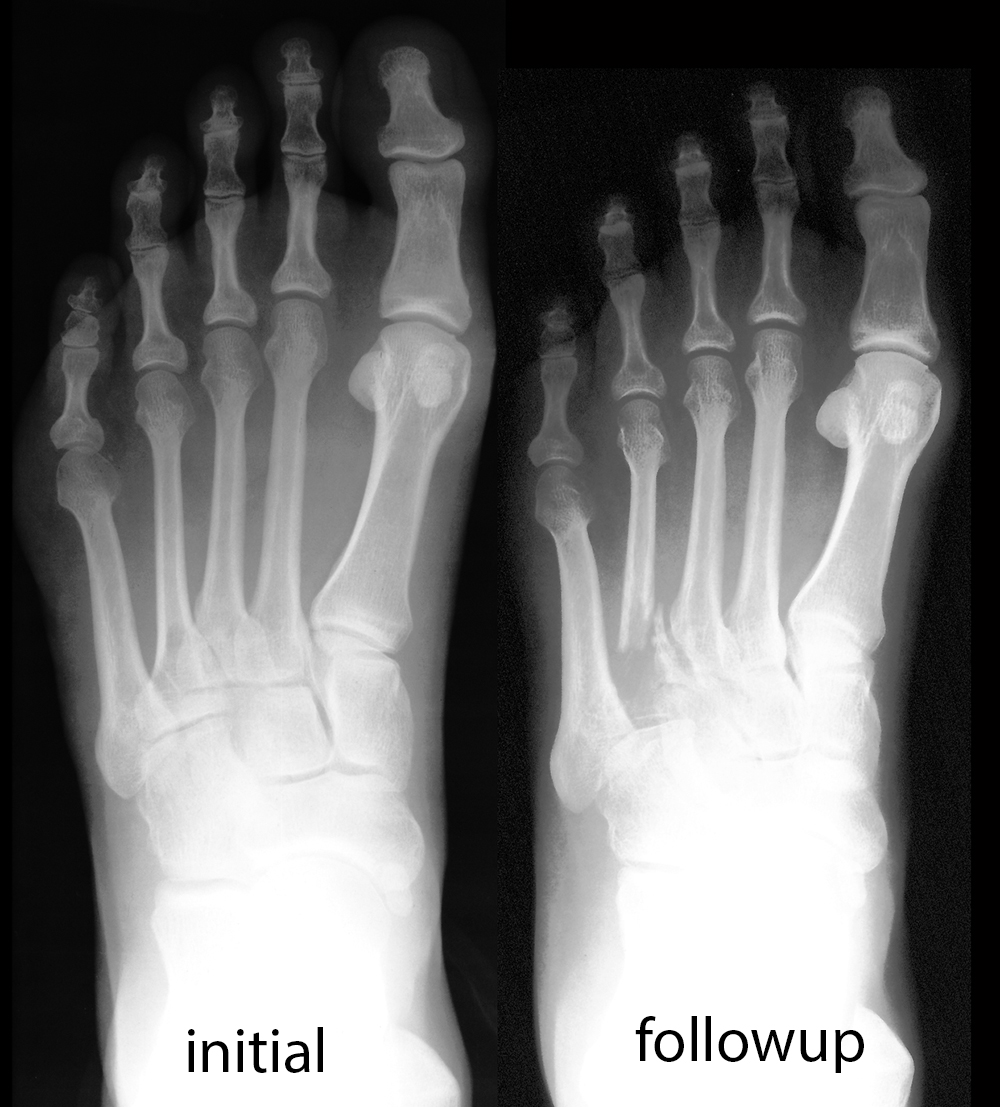
Case 1
Here are initial and followup studies done on this patient.
Question 12:
a) What are these studies?
These are both radiographs, in this case they are AP views of the foot.
b) Try to identify what is abnormal before clicking the link below.
On the initial image, which was read as normal, there is just a hint of lucency in the region of the base of the 4th metatarsal. This is where the patient's pain was located, and this corresponds to the area of abnormal uptake on later bone scan. Unfortunately, this was a metastasis from his lung cancer, and on the later image, the process has progressed, with a much larger lucent area and a pathologic fracture through the area of weakened bone. Bone scanning, despite the low resolution of the images, is very sensitive to abnormal processes like this. Bone scans can detect tumor, infection or fracture that may be missed with other types of imaging.