




Case 2
This is an imaging study on a 23 year old male with left testicular pain and a feeling of heaviness.
Question 1:
a) What is this imaging study?
This is a testicular ultrasound.
b) What are two advantages of this type of imaging compared to radiography (X-rays)?
Ultrasound does not involve radiation, and it is quick and easy to perform, including portably. It give real-time images so that you can check movement or changes over time, including providing guidance for biopsy or CVL (central venous line) placement or other procedures.
c) What are two limitations of this type of imaging?
The depth of penetration within body tissues is limited, and is less for higher resolution transducers, so there is a trade-off of image quality and depth of visualization. The sound beam is blocked by bone or air, which can limit the ability to image certain organs. The field of view is generally quite small, so it can make structures hard to identify, including normal anatomy. The image resolution is low, so the images are grainy.
Question 2:
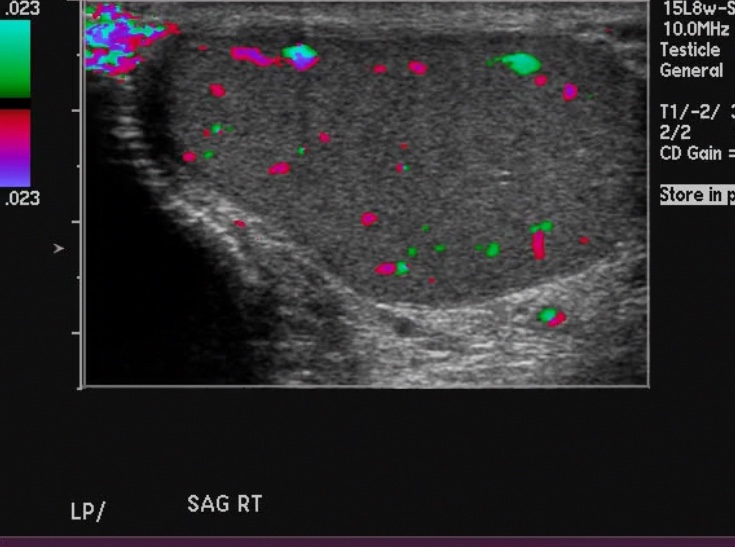
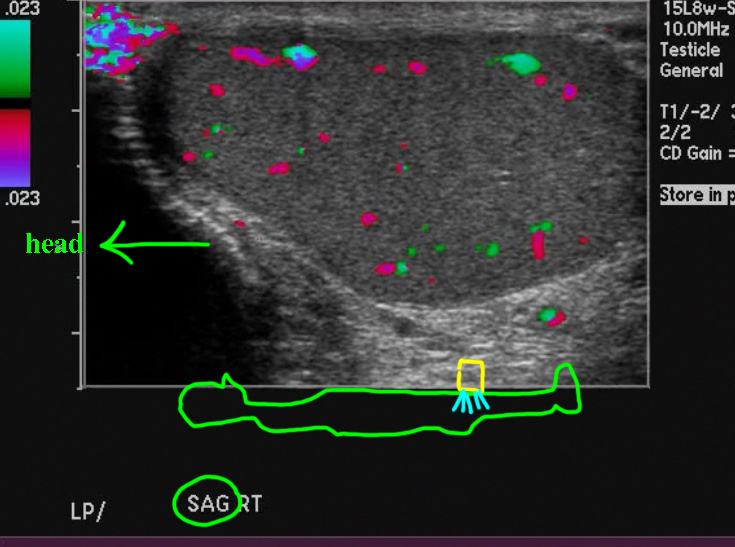
a) What specific imaging is shown on this selected image from the patient's ultrasound study?
This is a Doppler image showing flow within the region, demonstrated on a scale from purple to blue.
b) Is this image normal?
Yes, this is a normal appearance of scattered flow within the right testis.
c) What is the orientation of this image?
It is labeled 'SAG', meaning sagittal. By contention when we are doing sagittal imaging with ultrasound, the head is shown to the left side of the image. Check the 'orientation' link below to see a demonstration of this.
d) What structure is outlined in green when you click the link below?
This structure is the head of the epididymis, since it is to the left or head side of the image. It is very vascular, which is normal.
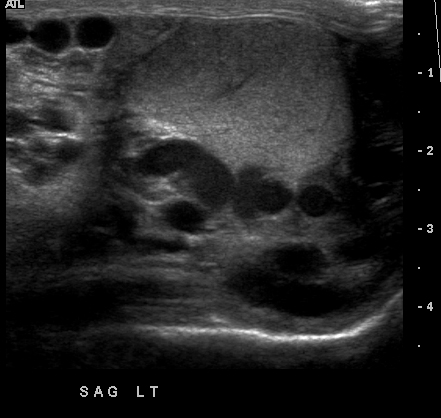
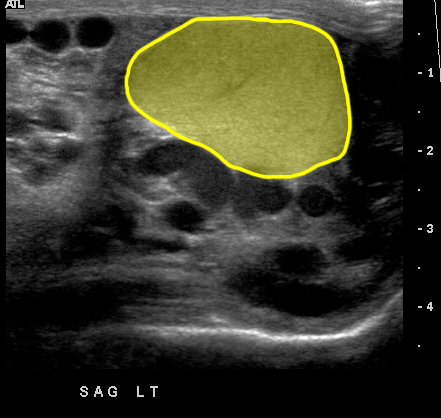
Case 2
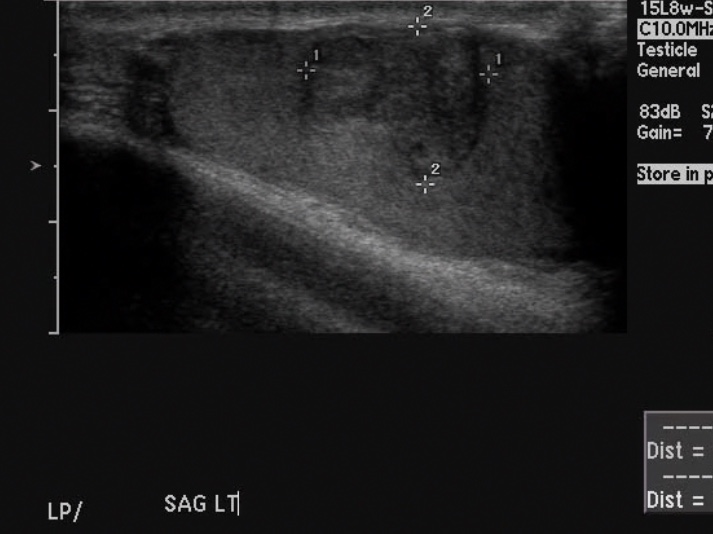
This is a view of the left testicle, which is the side with pain and a sensation of heaviness.
Question 3:
a) How would you describe the appearance of the left testicle?
If you click the link below, you can see that there is an irregular area of darker appearance (hypoechoic) that is also somewhat heterogeneous, compared to the very uniform appearance of normal testicular tissue.
b) What is the most likely diagnosis?
This is very worrisome for testicular carcinoma, which can occur in young patients, and typically presents with either a lump, pain, or both.

Case 2
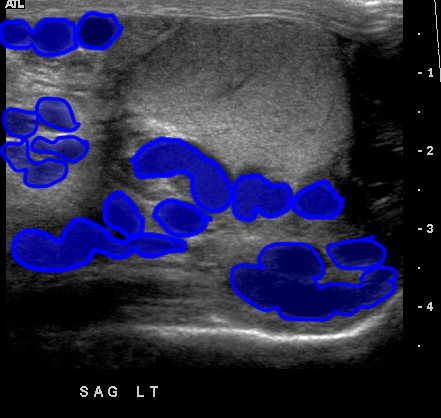
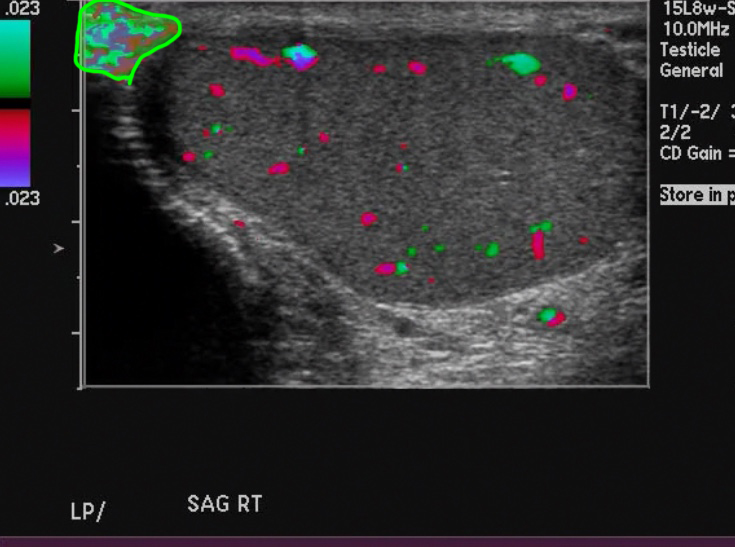
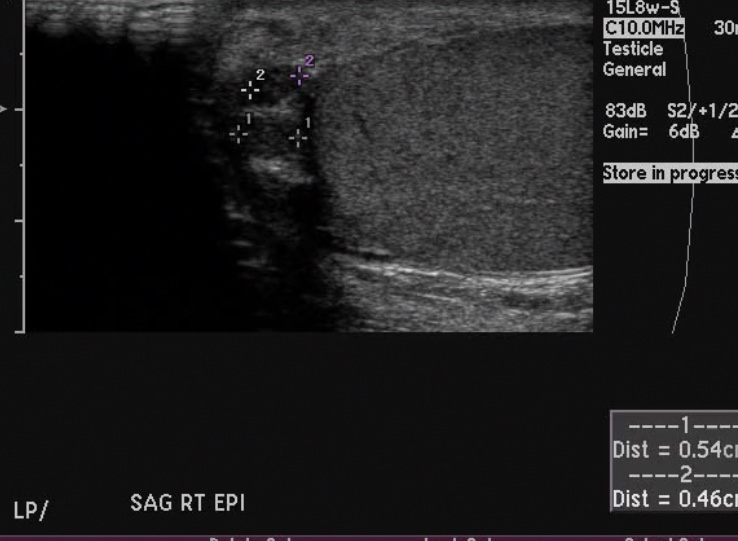
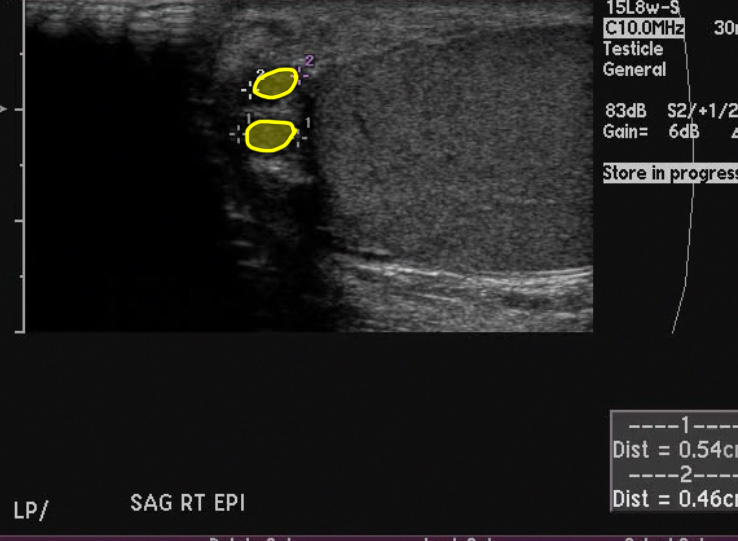
This is another image of the upper right testis.
Question 4:
How would you describe these findings in terms of shape and echogenicity?
The findings indicated by clicking the link below, are round, smooth, very dark areas in the region of the head of the epididymis. These are very common small fluid-filled collections called epididymal cysts or spermatoceles, depending on whether they contain just fluid or fluid and sperm. They are not concerning and need no treatment.
Case 2
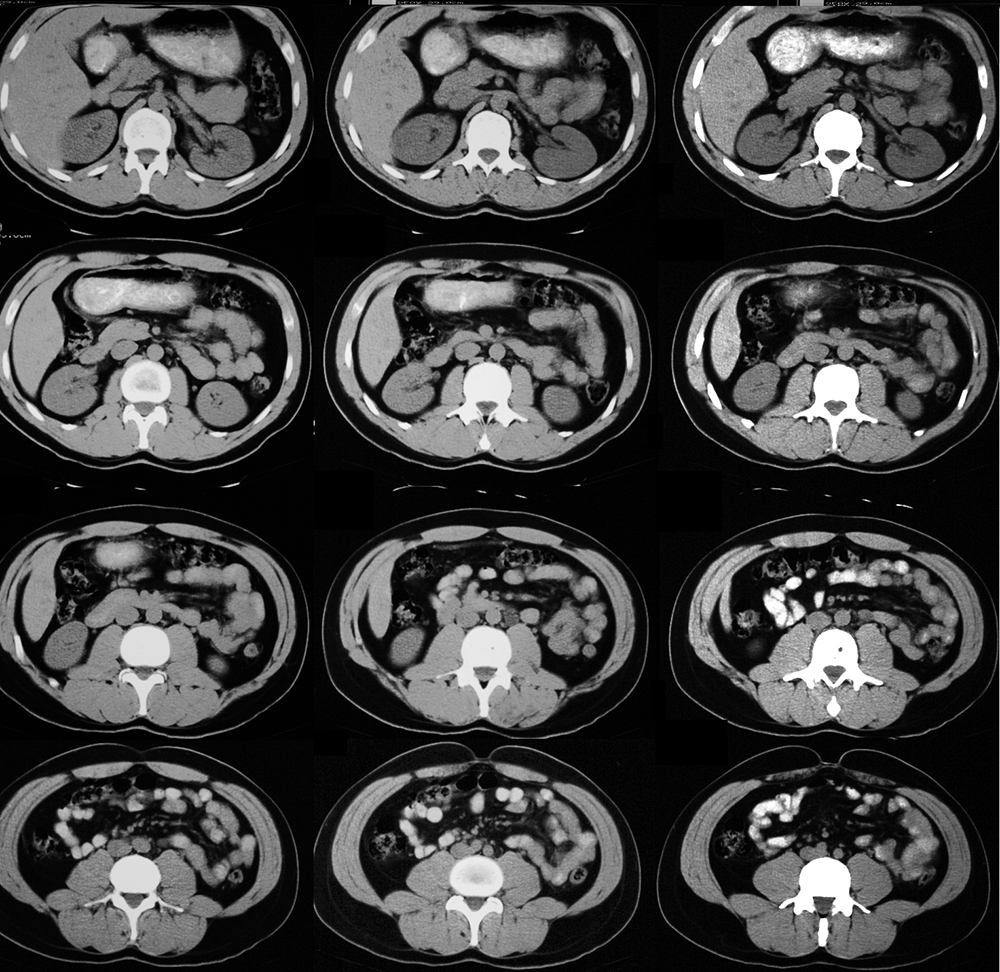
This is the next study that was done on this patient.
Question 5:
a) What is this study? Be specific.
This is a CT scan (cortical bone is white), in the axial plane, displayed with soft tissue windows (fat and muscle are very different in terms of their shades of grey), with oral but without intravenous contrast (vessels and muscle are the same shade of grey).
b) What is the vascular supply to the testis?
The gonadal arteries arise from the abdominal aorta, just below the level of the renal arteries, and travel down on the surface of the psoas muscles to reach the inguinal canal, passing alongside the vas deferens to reach the testis. The gonadal vein on the right drains into the IVC, but on the left drains into the left renal vein. These vessels are too small to be easily seen on these CT images. Click the link below to see the aorta and SMA/IMA outlined, as well as the IVC and the right and left renal veins.

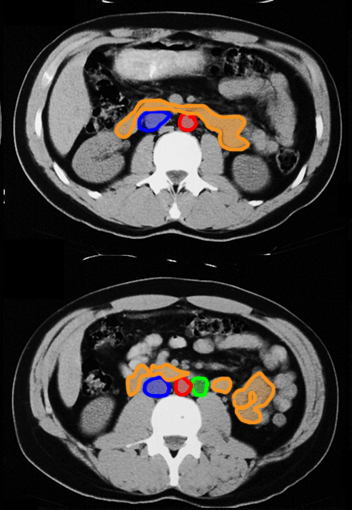
Case 2
These are two of the images from the previous CT scan.
Question 6:
a) Why is an understanding of the vascular supply of an organ important to track the likely sites of metastatic spread from a tumor?
For tumors that spread along lymphatic routes (as many do, including testicular cancer in some cases), the enlarged nodes will be alongside the vessels. In the case of the testis, the first nodes that are usually involved are not in the scrotum or pelvis but in the central abdomen, near or just below the renal vessels. An abnormal enlarged node is shown below in this patient which represents spread of his testicular tumor.
b) What are the outlined structures on the image labeled 'abnormal node'?
red = aorta blue = IVC green = enlarged node (metastasis from testicular tumor) orange = adjacent bowel loops, mostly duodenum and proximal jejunum

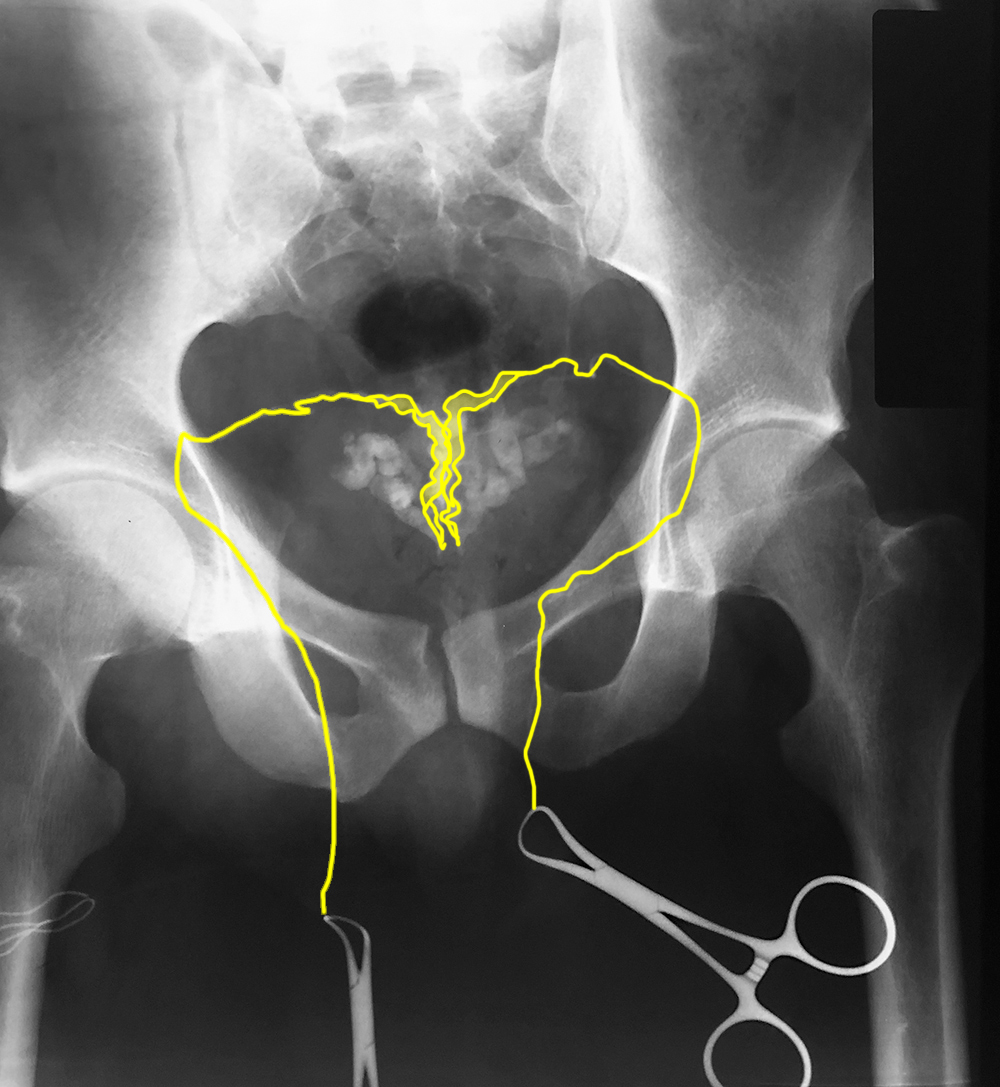
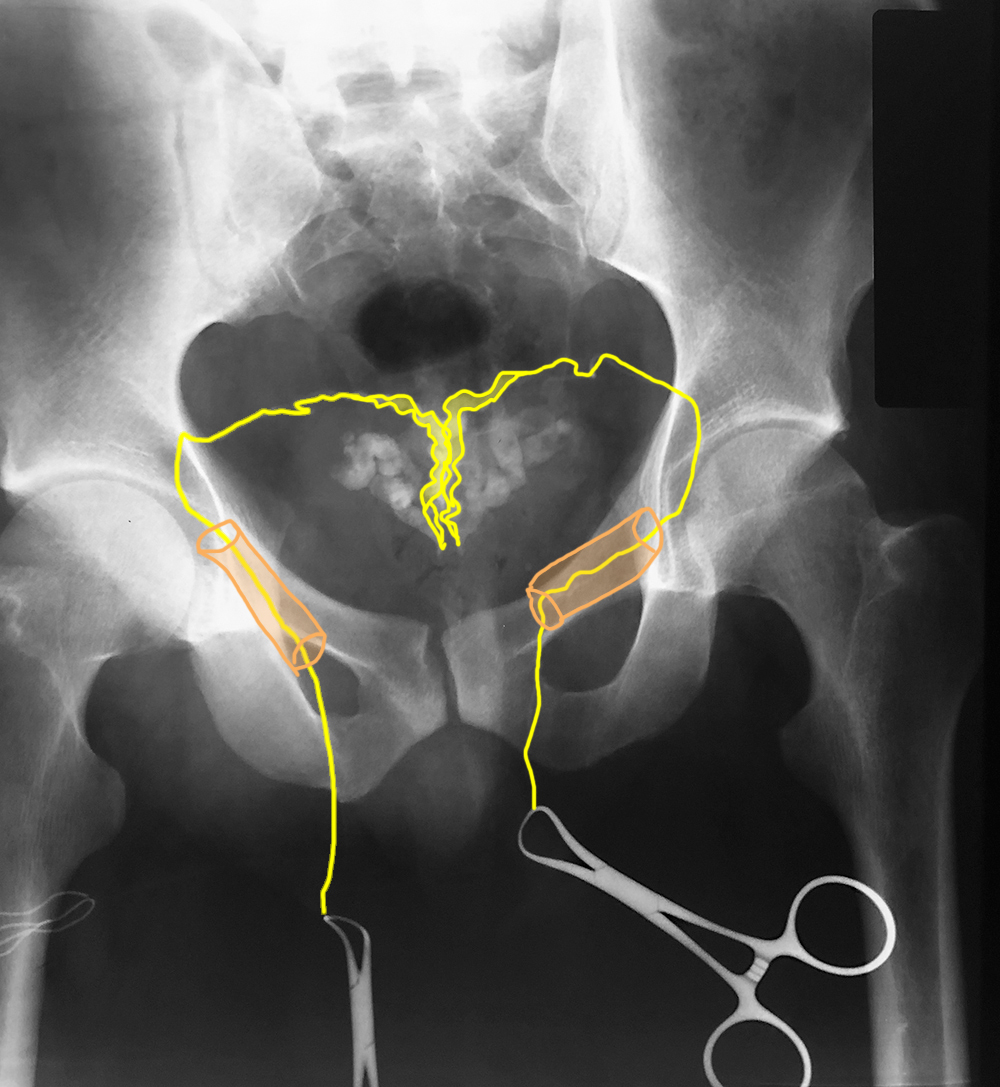
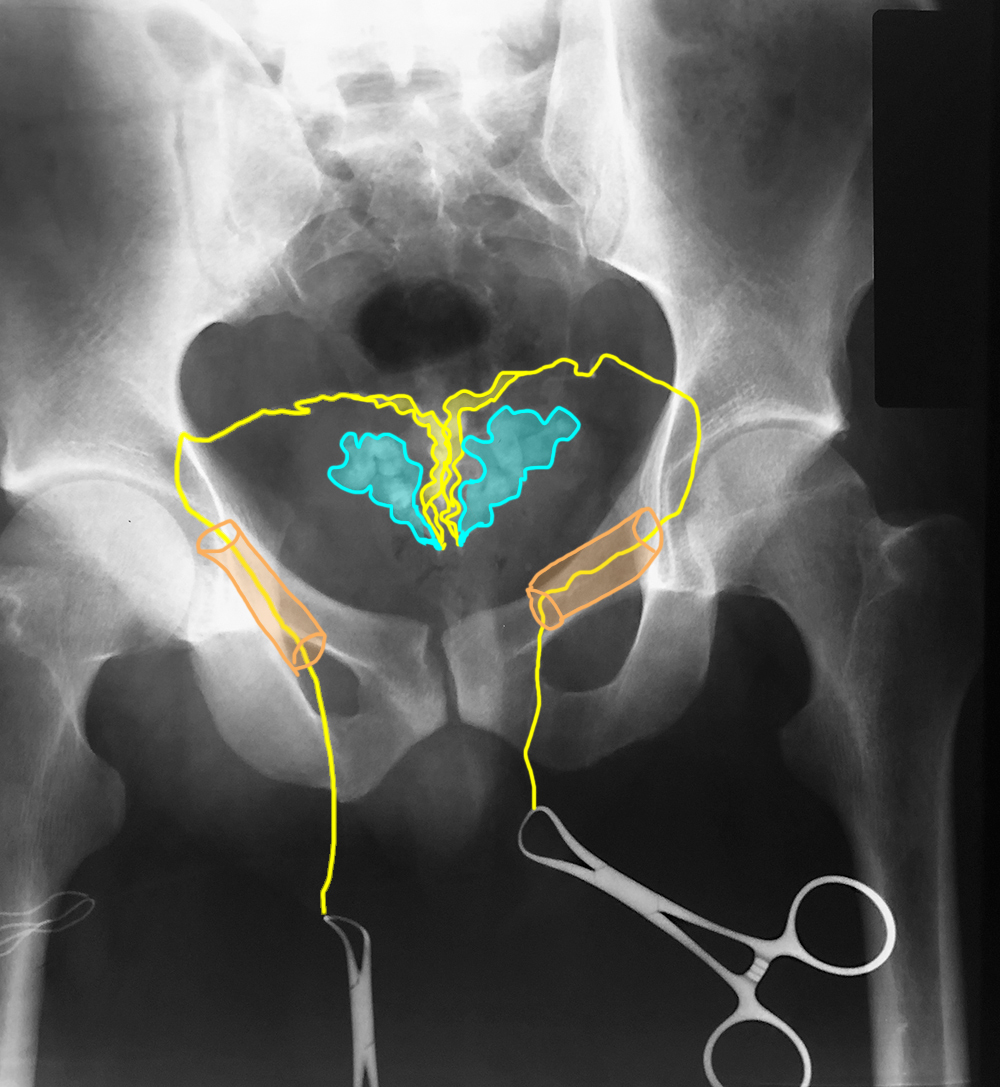
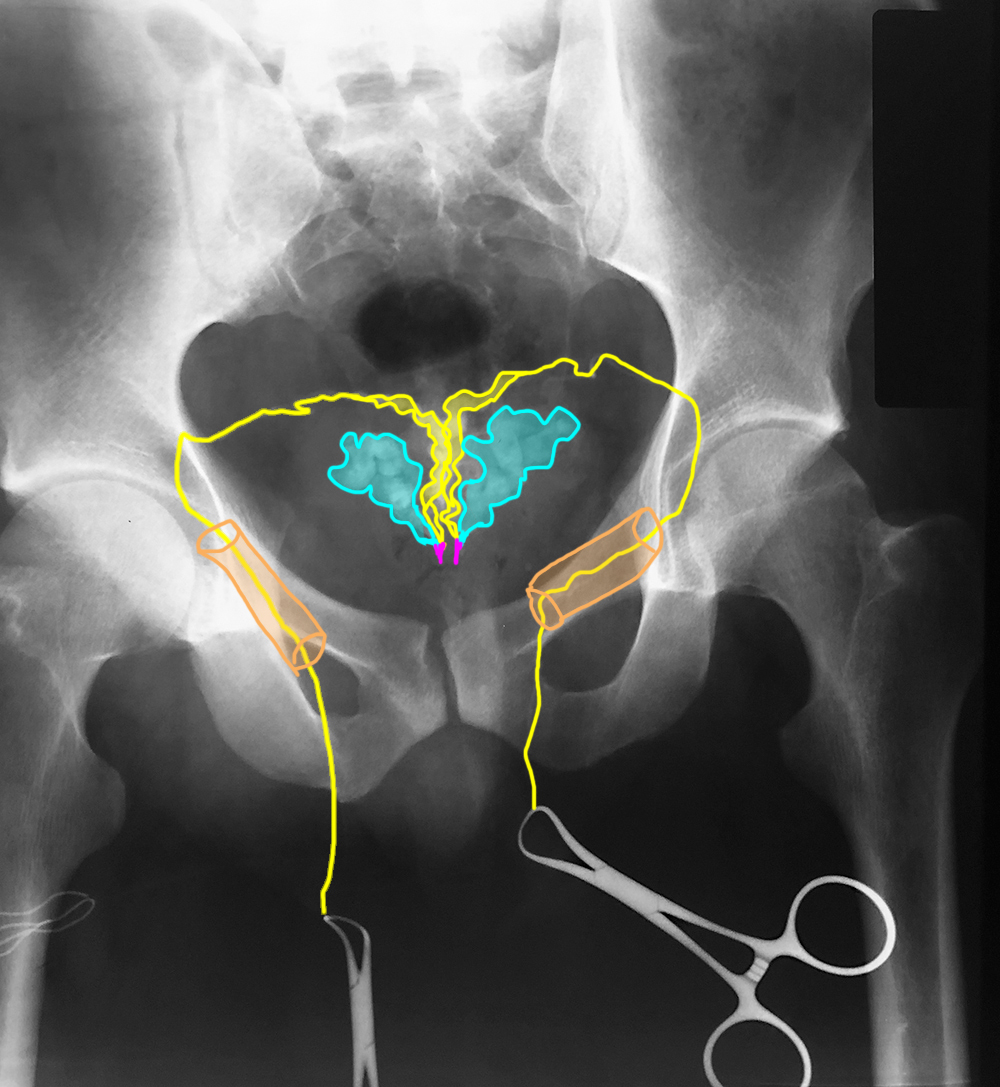
Case 2
This is a study done in a different patient with infertility, but testicular biopsy showing normal sperm formation in the testis. Try to identify the different parts of the male genital tract from the vas proximally before clicking the links below. This study is normal.
Question 7:
How was this study done?
This is a vasogram, done by isolating the vas deferens in the scrotum and injecting contrast material through a small incision, flowing back along the vas and into the other male pelvic organs, to check for continuity or blockage.

Case 2
This is another young patient with painless swelling in the left scrotum.
Question 8:
a) What is this study?
This is another testicular ultrasound with Doppler.
b) What looks abnormal?
There are many round and curving tubular anechoic (totally black) structures in the left scrotum, outside the testis. They are bright on Doppler indicating that there is flow within them consistent with vessels. It is unusual for arteries to become this dilated and tortuous so they are most likely enlarged veins.
Case 2
This is a single image from the patient's ultrasound study.
Question 9:
a) Do you think the testis looks normal or abnormal?
The testis looks normal, with a uniform mid-range grey texture and no masses.
b) What is this condition called?
This is called a varicocele, and is a common abnormality often associated with infertility.
c) Is there an anatomic reason why this might be more common on the left than the right?
It is thought that the more complicated course of the left testicular vein, draining into the left renal vein at a right angle, compared to the right testicular vein (that drains at an oblique angle directly into the IVC) likely explains potential increased pressure on the left and higher likelihood of developing dilated veins.